Translate this page into:
Factors associated with uncontrolled asthma among Sudanese adult patients
*Corresponding author: Rashid Osman, Department of Lung Health, The Epidemiological Laboratory for Research and Public Health, Khartoum, Sudan. rashildo@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Osman R, Ahmed K, ElSony A. Factors associated with uncontrolled asthma among Sudanese adult patients. J Pan Afr Thorac Soc 2021;2(2):85-93.
Abstract
Objectives:
Uncontrolled asthma is a major health problem resulting in increased morbidity, mortality, healthcare utilization, and costs. The aim of this study was to determine the level of asthma control and its associated factors in Sudan.
Materials and Methods:
We performed a cross-sectional study of 362 adult asthmatics consecutively recruited from the three main tertiary hospitals in Khartoum State-Sudan, between March and June 2018. Data were collected using standardized questionnaires and the asthma control test (ACT) was used to determine the level of control. Logistic regression analysis was used to determine factors associated with uncontrolled asthma.
Results:
The mean age of the subjects was 40.1 years (SD 15.7) and the sex distribution was almost equal, with 195 (53.9%) females. Among all asthmatics, the prevalence of uncontrolled asthma was 84.5%, according to ACT score. Factors associated with uncontrolled asthma included; health facility (odd ratios [OR] = 2.96 [1.27–6.86]), time to reach facility (OR = 4.51 [1.68–12.06]), non-adherence to follow-up visits (OR = 5.11 [1.12–23.36]), steroids tablets use without prescription (OR = 9.01 [1.01–79.88]), family history of asthma (OR = 0.45 [0.21– 0.95]), and inhaler technique training (OR = 0.37 [0.17–0.78]).
Conclusion:
This study showed a high rate of uncontrolled asthma in three tertiary hospitals in Khartoum. Factors associated with uncontrolled asthma may be considered as targets for future intervention strategies.
Keywords
Asthma
Chronic respiratory disease
Asthma control
Middle East and North Africa
Low- and middle-income countries
INTRODUCTION
Asthma constitutes a significant public health problem and its burden is high in both developed and developing countries. Recent estimates suggest that 358 million people globally have asthma and the prevalence has increased by 12.6% in 2015 compared to 1990.[1] There will be an additional 100 million people with asthma by 2025, mostly due to the projected increase in urban population. In Khartoum, the capital of Sudan, asthma prevalence ranged from 12.5% in children[2] to 10.8% in adults.[3]
In most European countries, asthma-related hospitalizations recently declined, with an over two-fold reduction in some countries.[4] While in Sudan, asthma is the fifth-highest cause of hospitalizations after pneumonia, malaria, diarrheal diseases, and diabetes.[5] In addition, general hospitals have witnessed a dramatic increase in the number of emergency room (ER) visits by asthma patients in previous years.[6]
Asthma morbidity is high in low-and middle-income countries (LMICs) since most patients have poor or limited access to healthcare and essential medicines.[7] Most of the asthma patients seen in general practice have uncontrolled symptoms and poor knowledge and skills in asthma management, medication use, and inhaler technique.[8] Poor asthma control is related to increased morbidity, healthcare utilization, healthcare costs, and mortality. Poor awareness and knowledge about asthma guidelines, suboptimal infrastructure, and diagnostic facilities[9] as well as non-availability and high cost of asthma medications are among the health system factors that are associated with poor asthma control in LMICs.[10] Patient-related factors such as sociodemographics, asthma education, active and passive smoking,[11,12] adherence to medications and follow-up visits, and personal beliefs regarding asthma may influence asthma control.
In Sudan, despite the local adaptation of international guidelines and piloting asthma standard case management (SCM) proposed by the International Union against Tuberculosis and Lung Diseases (The UNION) which substantially reduced symptoms severity, ER visits, and hospitalizations,[6] a recent study reported that the majority of asthma patients (58%) seen at referred clinics in Khartoum were not receiving medications as recommended by the international asthma guidelines.[13]
Asthma control data from LMICs are scarce, and it is difficult to generalize data obtained in other parts of the world to specific ethnic and social contexts. Nevertheless, there is reasonable information on the level of asthma control from several countries in the Middle East and North Africa (MENA), but data from Sudan are lacking and the factors associated with asthma control are not well studied.
We conducted a study to determine the level of asthma control among patients attending tertiary hospitals in Khartoum and to identify the factors which may influence asthma control.
MATERIALS AND METHODS
Setting
The present study was conducted at the outpatient clinics of three main tertiary hospitals (Ibrahim Malik, Khartoum North, and Omdurman) in Khartoum. Khartoum is the most populated state, with a population of eight million people approximately.[5] The population is a mixture of all Sudanese tribes and ethnic groups. Khartoum is geographically divided into three regions, namely Khartoum, Khartoum-North, and Omdurman. Health services are available in private and governmental forms. Apart from the private sector, there are 48 governmental hospitals, 236 health centers, and 146 dispensaries.[5]
Design and aims
This was a cross-sectional hospital-based study in which all asthmatics presenting at the outpatient clinics were sequentially included to identify the level of asthma control and associated factors.
Population
All potential asthma patients were recruited from the three randomly selected healthcare facilities between March and June 2018. Patients had to be aged ≥18 years, reported to have a physician diagnosis of asthma clinically or by lung function testing, and have been prescribed asthma medications. Patients were excluded if they had attended the clinic for <3 months, or had been diagnosed with chronic pulmonary diseases other than asthma such as chronic obstructive pulmonary disease, emphysema, chronic bronchitis, bronchiectasis, or did not have complete data on questionnaires. Recruitment continued in this way until the desired sample was met.
Data collection
Data were collected using a structured interviewer-administered questionnaire which includes the patient’s sociodemographic information and patient-related factors such as duration of asthma symptoms, number of ER visits and hospitalizations, asthma medications, adherence to medications (assessed by answering to; How often do you use your medication as prescribed?) and adherence to follow-ups visits (assessed by answering to; Have you been asked to come for follow up visit in the past 12 months, if yes how often do you come for follow-up?), and receiving training on inhalation technique (answered yes or no to; Have you had any inhaler technique training?).
Assessment of asthma control
Asthma control was assessed using a validated tool, the asthma control test (ACT).[14] The ACT is a self-completed questionnaire comprising five questions that assess activity limitation, shortness of breath, nighttime symptoms, use of rescue medication, and patient rating of asthma control over the previous 4 weeks. The questions are scored from 1 (worst) to 5 (best), and the ACT score is the sum of the responses, with a maximum best score of 25. A score of ≥20 is the optimal cutoff point of well-controlled asthma over the previous 4 weeks.[14] A validated, published, and Arabic version of the ACT[15] was used to assess asthma control for this study.
Data entry and quality control
Before the study commencement, questionnaires were pretested in five asthma patients from each facility and changes were made as appropriate. The interviewers were trained in the questionnaire administration. Data were then cleaned, corrected for completeness and correctness, double-entered, and cross-checked. Every patient was given a single defined code.
Study size
Based on the proportion of patients inadequately receiving medications (58%) earlier reported in Sudan,[13] the calculated sample size was 374 participants. This formula was used to determine the sample size. n = Z2PQ/D2, where n = sample size, Z = 1.96, P = population proportion estimated from previous study, Q = 100-p, Z = confidence level at 95% (1.96), and D = desired marginal error (0.05).
Data analysis
Descriptive statistics were used to describe the basic characteristics of the study participants. Means and standard deviations (SDs) were calculated for normally distributed continuous variables, whereas proportions with 95% confidence intervals (CIs) were calculated for the categorical variables. The median and the interquartile range (IQR) were calculated for continuous variables with the asymmetric distribution. Pearson’s Chi-square test or the Fisher’s exact test was used to test for associations between each independent variable and asthma control. Logistic regression was used to identify factors associated with uncontrolled asthma (ACT score ≤ 19) and to calculate the odds ratio (OR) and 95% CI. Univariate analysis was conducted for every variable alone, and statistically significant results (P < 0.05) were then included together in the multivariate model. The data were processed and analyzed by the Statistical Package for the Social Sciences software (SPSS, version 20, IBM, Armonk, NY, USA).
Ethics statement
The study was approved by the National Research Ethics Review Committee at the Ministry of Health, Khartoum Sudan (Serial Number; KMOH-REC-2-2020) and the Institutional Review Board at Alneelain University, Khartoum, Sudan. All participants were given information about the study and provided written informed consent.
RESULTS
Participants
Of 394 potential asthma patients approached at the outpatient’s clinics of the three hospitals, only 374 (94.92%) gave consent and completed the questionnaires. Seven participants were excluded from the study because their asthma diagnosis was not previously confirmed by a physician. Another five participants were excluded from the analysis because they had incomplete data [Figure 1].
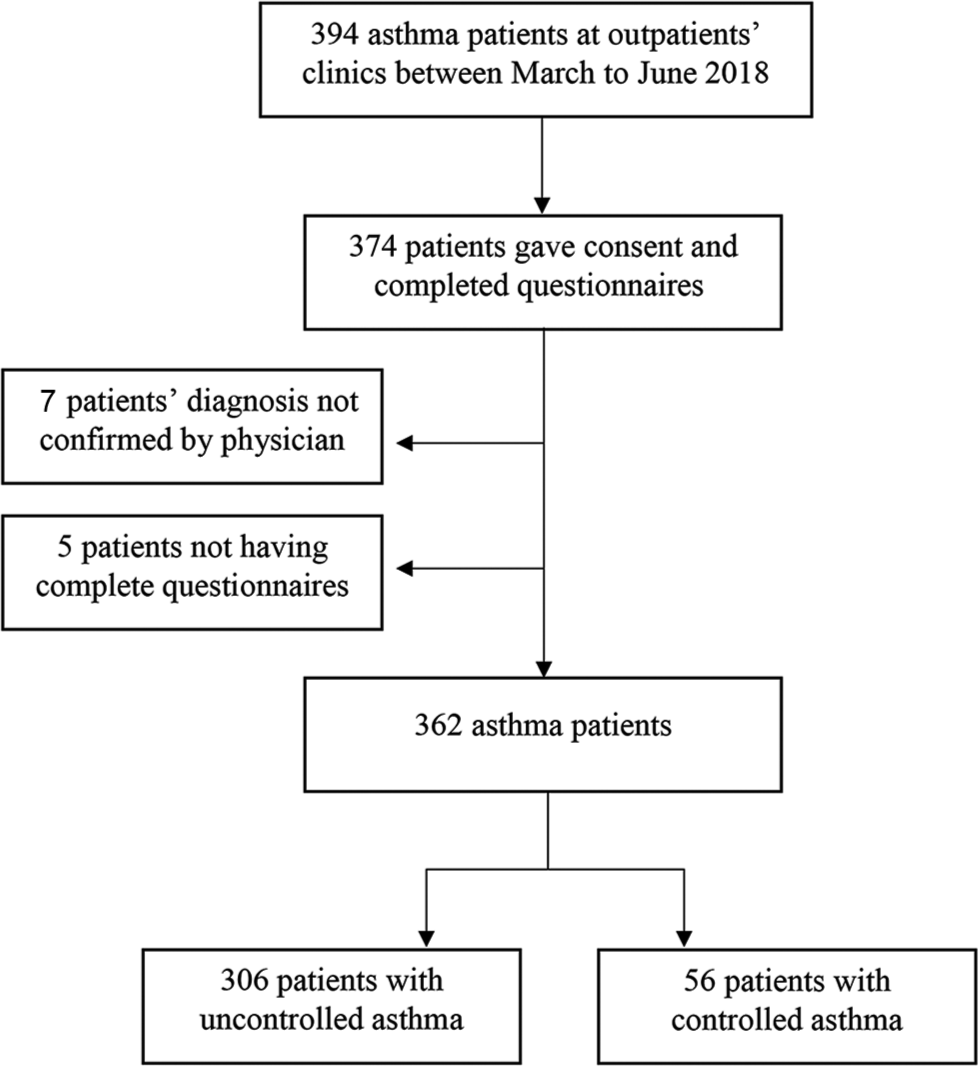
- Flow chart of the study sample. Based on asthma control test (ACT), a score ≤19 indicated “uncontrolled” asthma and a score ≥20 indicated “controlled” asthma.
Sociodemographic characteristics
The mean age of the study participants was 40.1 years (±15.7) and the sex distribution was almost equal with 53.9% females. More than half of the participants (55.2%) were married and only 24.9% graduated from university. The majority of participants were of rural origin (56.7%). Most of the participants were either employed staff or workers (59.1%) and only 37.8% were health insured.
Clinical profile
The majority of the participants (60.5%) had asthma symptoms for more than 5 years, with a median of 9 years (IQR = 3–16). Almost a third (31.5%) had asthma since childhood and 45.6% had a family history of asthma. Medications used were mainly inhaled salbutamol (47.8%), budesonide-fluticasone combination (24.9%), or both (23.2%). Steroids tablets without prescription were used by 27.1%. Only 43 (11.9%) of the participants had comorbidity, mainly hypertension in 22 subjects and 4.4% were current smokers. Patients who had undergone peak flow meter measurement were 15.7% and those who had been diagnosed using spirometry were only 12.4%.
Asthma control
Based on the ACT scores, uncontrolled asthma was present in 306 (84.5%) patients, with a mean ACT score of 13.58 (±3.27) among the uncontrolled compared to 21.57 (±1.17) in the controlled asthma patients.
Association between sociodemographic characteristics and asthma control
All the studied variables of the sociodemographic characteristics were not significantly associated with asthma control [Table 1].
| Asthma control* | Total n (%) | P-value# | ||
|---|---|---|---|---|
| Uncontrolled n (%) | Controlled n (%) | |||
| Age | ||||
| 18–29 years | 95 (84.1) | 18 (15.9) | 113 (100) | 0.31 |
| 30–44 | 97 (82.9) | 20 (17.1) | 117 (100) | |
| 45–59 | 63 (81.8) | 14 (18.2) | 77 (100) | |
| ≥60 | 51 (92.7) | 4 (7.3) | 55 (100) | |
| Gender | ||||
| Male | 141 (84.4) | 26 (15.6) | 167 (100) | 0.96 |
| Female | 165 (84.6) | 30 (15.4) | 195 (100) | |
| Marital status | ||||
| Single | 101 (79.5) | 26 (20.5) | 127 (100) | 0.10 |
| Married | 177 (88.5) | 23 (11.5) | 200 (100) | |
| Divorced | 15 (75.0) | 5 (25.0) | 20 (100) | |
| Widowed | 13 (86.7) | 2 (13.3) | 15 (100) | |
| Residence | ||||
| Urban | 136 (86.1) | 22 (13.9) | 158 (100) | 0.47 |
| Rural | 170 (83.3) | 34 (16.7) | 202 (100) | |
| Education | ||||
| Illiterate | 40 (83.3) | 8 (16.7) | 48 (100) | 0.40 |
| Primary | 86 (81.9) | 19 (18.1) | 105 (100) | |
| Secondary | 103 (86.9) | 16 (13.4) | 119 (100) | |
| University-graduate | 68 (84.0) | 13 (16.0) | 81 (100) | |
| Post-graduate | 9 (100.0) | 0 (0.0) | 9 (100) | |
| Occupation | ||||
| Housewife | 88 (83.8) | 17 (16.2) | 105 (100) | 0.27 |
| Worker | 97 (80.8) | 23 (19.2) | 120 (100) | |
| Employee | 80 (85.1) | 14 (14.9) | 94 (100) | |
| Student | 40 (95.2) | 2 (4.8) | 42 (100) | |
| Unemployed | 1 (100.0) | 0 (0.0) | 1 (100) | |
| Household monthly income | ||||
| <1000 SDP | 107 (90.7) | 11 (9.3) | 118 (100) | 0.10 |
| 1001–2000 | 95 (79.2) | 25 (20.8) | 120 (100) | |
| 2001–3000 | 78 (84.8) | 14 (15.2) | 92 (100) | |
| >3000 | 26 (81.2) | 6 (18.8) | 32 (100) | |
Association between health-related factors and asthma control
Factors associated significantly with asthma control were; health facility where health care was accessed (P = <0.001), time to reach health facility (P = 0.01), asthma duration (P = 0.01), family history of asthma (P = <0.001), hospitalizations (P = <0.001), previous ICU admission (P = <0.01), adherence to follow-up visits (P = 0.01), adherence to medication (P = 0.04), steroid tablets use without prescription (P = 0.03), avoidance of asthma triggers (P = 0.01), and receiving inhaler technique training (P = <0.001) [Table 2].
| Asthma control* | Total n (%) | P-value# | ||
|---|---|---|---|---|
| Uncontrolled n (%) | Controlled n (%) | |||
| Health facility | ||||
| Ibrahim Malik | 69 (75.0) | 23 (25.0) | 92 (100) | <0.001 |
| Omdurman | 119 (92.2) | 10 (7.8) | 129 (100) | |
| Khartoum North | 118 (83.7) | 23 (16.3) | 141 (100) | |
| Distance from health facility | ||||
| <5 km | 135 (82.3) | 29 (17.7) | 164 (100) | 0.06 |
| 5–10 km | 109 (90.8) | 11 (9.2) | 120 (100) | |
| >10 km | 62 (79.5) | 16 (20.5) | 78 (100) | |
| Time to reach health facility | ||||
| <15 min | 123 (86.0) | 20 (14.0) | 143 (100) | 0.01 |
| 15–30 min | 148 (87.6) | 21 (12.4) | 169 (100) | |
| >30 min | 35 (70.0) | 15 (30.0) | 50 (100) | |
| Asthma duration | ||||
| <2 year | 50 (73.5) | 18 (26.5) | 68 (100.0) | 0.01 |
| 2–5 year | 61 (81.3) | 14 (18.7) | 75 (100) | |
| >5 year | 195 (89.0) | 24 (11.0) | 219 (100) | |
| Family history of asthma | ||||
| Yes | 149 (90.3) | 16 (9.7) | 165 (100) | <0.001 |
| No | 157 (79.7) | 40 (20.3) | 197 (100) | |
| Smoking | ||||
| Yes current | 12 (75.0) | 4 (25.0) | 16 (100) | 0.53 |
| Ex-smoker | 40 (83.3) | 8 (16.7) | 48 (100) | |
| No never | 254 (85.2) | 44 (14.8) | 298 (100) | |
| ER visits | ||||
| 1–3 | 119 (87.5) | 17 (12.5) | 136 (100) | 0.46 |
| 4–6 | 72 (83.7) | 14 (16.3) | 86 (100) | |
| >6 | 115 (82.1) | 25 (17.9) | 140 (100) | |
| Hospitalizations | ||||
| Non | 193 (77.8) | 55 (22.2) | 248 (100) | <0.001 |
| 1–3 | 92 (98.9) | 1 (1.1) | 93 (100) | |
| >3 | 21 (100.0) | 0 (0.0) | 21 (100) | |
| ICU or ventilation | ||||
| Yes | 72 (94.7) | 4 (5.3) | 76 (100) | <0.001 |
| No | 234 (81.8) | 52 (18.2) | 286 (100) | |
| Adherence to follow-up visits | ||||
| Always | 66 (95.7) | 3 (4.3) | 69 (100) | 0.01 |
| Often | 68 (87.2) | 10 (12.8) | 78 (100) | |
| Sometimes | 105 (80.2) | 26 (19.8) | 131 (100) | |
| Rarely | 42 (85.7) | 7 (14.3) | 49 (100) | |
| Never | 25 (71.4) | 10 (28.6) | 35 (100) | |
| Adherence to medications | ||||
| Always | 149 (89.8) | 17 (10.2) | 166 (100) | 0.04 |
| Often | 53 (79.1) | 14 (20.9) | 67 (100) | |
| Sometimes | 74 (77.9) | 21 (22.1) | 95 (100) | |
| Rarely | 19 (82.6) | 4 (17.4) | 23 (100) | |
| Never | 11 (100.0) | 0 (0.0) | 11 (100) | |
| Steroids use without prescription | ||||
| Non | 216 (81.8) | 48 (18.2) | 264 (100) | 0.03 |
| 1–3 | 54 (88.5) | 7 (11.5) | 61 (100) | |
| >3 | 36 (97.3) | 1 (2.7) | 37 (100) | |
| Asthma triggers avoidance | ||||
| Always | 97 (82.9) | 20 (17.1) | 117 (100) | 0.01 |
| Often | 75 (92.6) | 6 (7.4) | 81 (100) | |
| Sometimes | 105 (79.5) | 27 (20.5) | 132 (100) | |
| Rarely | 26 (96.3) | 1 (3.7) | 27 (100) | |
| Never | 3 (60.0) | 2 (40.0) | 5 (100) | |
| Inhaler technique trained | ||||
| Yes | 259 (88.4) | 34 (11.6) | 293 (100) | <0.001 |
| No | 47 (68.1) | 22 (31.9) | 69 (100) | |
In the univariate analysis, eight factors were associated with asthma control; the health facility, time to reach facility, asthma duration, previous ICU admission, steroids tablets use without prescription, adherence to follow-up visits, family history of asthma, and previous inhaler technique training [Table 3]. In the multivariate analysis, six factors remained significantly associated with uncontrolled asthma; health facility, longer time to reach facility, steroids tablets use without prescription, non-adherence to follow-up visits, family history of asthma and previous inhaler technique training. The health facility where health care was accessed; patients attending Ibrahim Malik hospital were more likely to have uncontrolled asthma compared to those attending Khartoum-North hospital (aOR = 2.96 [1.27–6.86]). Longer time to reach facility; those who took more than 30 min were more likely to have uncontrolled asthma than patients who took <15 min to reach the nearest health facility (aOR = 4.51 [1.68–12.06]). Steroids tablets use without prescription; those who used steroids were more likely to have uncontrolled asthma (aOR = 9.01 [1.01–79.88]). Non-adherence to follow-up visits; patients who had never come to follow-up visits were more likely to have uncontrolled asthma compared to those who had always come to follow-up (aOR = 5.11 [1.12–23.36]). Family history of asthma; those who had family history of asthma were less likely to have uncontrolled asthma compared to those who had not (aOR = 0.45 [0.21–0.95]). Previous inhaler technique training; patients who had received training on inhaler technique were less likely to have uncontrolled asthma compared to those who had not (aOR = 0.37 [0.17–0.78]) [Table 3].
| Factors | Unadjusted m OR (95 CI) | P-value | Adjusted OR (95 CI) | P-value |
|---|---|---|---|---|
| Health facility | ||||
| Khartoum North | ||||
| Ibrahim Malik | 1.71 (0.89–3.27) | 0.11 | 2.96 (1.27–6.86) | 0.01 |
| Omdurman | 0.43 (0.19–0.95) | 0.03 | 0.48 (0.19–1.23) | 0.13 |
| Time to reach health facility | ||||
| <15 min | ||||
| 15–30 min | 0.87 (0.45–1.68) | 0.68 | 0.80 (0.36–1.73) | 0.55 |
| >30 min | 2.64 (1.22–5.68) | 0.01 | 4.51 (1.68–12.06) | <0.001 |
| Asthma duration | ||||
| <2 year | ||||
| 2–5 year | 2.92 (1.47–5.81) | <0.001 | 1.94 (0.83–4.51) | 0.12 |
| >5 year | 1.86 (0.91–3.83) | 0.09 | 1.11 (0.47–2.61) | 0.81 |
| Family history of asthma | ||||
| No | ||||
| Yes | 0.42 (0.22–0.78) | <0.001 | 0.45 (0.21–0.95) | 0.03 |
| ICU or Ventilation | ||||
| No | ||||
| Yes | 4.00 (1.39–11.44) | 0.01 | 2.92 (0.92–9.23) | 0.06 |
| Adherence to follow-up visits | ||||
| Always | ||||
| Often | 3.23 (0.85–12.28) | 0.08 | 2.69 (0.66–11.04) | 0.17 |
| Sometimes | 5.45 (1.58–18.71) | 0.01 | 5.24 (1.42–19.32) | 0.01 |
| Rarely | 3.67 (0.89–14.97) | 0.07 | 2.47 (0.51–11.79) | 0.25 |
| Never | 8.80 (2.23–34.62) | <0.001 | 5.11 (1.12–23.36) | 0.03 |
| Steroid tabs use | ||||
| Non | ||||
| 1–3 | 8.00 (1.07–59.79) | 0.04 | 9.01 (1.01–79.88) | 0.05 |
| >3 | 4.66 (0.55–39.55) | 0.15 | 8.45 (0.82–86.89) | 0.07 |
| Inhaler technique trained | ||||
| No | ||||
| Yes | 0.28 (0.15–0.52) | <0.001 | 0.37 (0.17–0.78) | <0.001 |
Reference group: First in any of the categorical variables, OR: Odds ratio, CI: Confidence interval, Km: Kilometer, min: Minutes, ICU: Intensive care unit
DISCUSSION
In this study from the MENA region, we found a very high prevalence of uncontrolled asthma (84.5%) among Sudanese adults attending three tertiary hospitals in Khartoum. We also found that the health facility, longer time to reach facility, steroids tablets use, non-adherence to follow-up visits, not having family history of asthma, and lack of training on inhaler technique were significantly associated with uncontrolled asthma.
Globally, several studies have also documented suboptimal asthma control. In population studies in five European countries, the prevalence of uncontrolled asthma was 53.5%.[16] In the United States, 58% of asthma patients have uncontrolled asthma.[17] In Latin America[18] and Asia-Pacific[19] and Nigeria,[20] Asthma Insights and Management surveys reported 93%, 92.4%, and 93.8% of partly-controlled or uncontrolled asthma in these regions. In the MENA,[21] uncontrolled asthma prevalence ranged from 57.4% to 85.2%, with an overall prevalence of 70.6% in 11 countries. In other African countries, including Cameroon, DR Congo, the Maghreb countries, and Ethiopia, studies have reported uncontrolled asthma prevalence of 42%, 56%, 71.3%, and 85.2%, respectively.[22-25]
This high prevalence of uncontrolled asthma in our study may be related to the location of the study in tertiary care hospitals where patients with more severe diseases are likely to attend. This high level of uncontrolled asthma may be linked to the underuse of the recommended prophylactic medications since only (24.9%) of the patients used them in this study.
To achieve good outcomes in asthma control, the GINA[26] and the UNION,[7] recommend improving the quality of services provided to asthma patients through implementation of asthma guidelines, use of diagnostic tools such as peak-flow-meter and spirometer, provision of affordable quality-assured medications, and regular training of health providers.
We found that the health facility and its available resources for asthma are associated with uncontrolled asthma. Patients attending Ibrahim Malik hospital were almost 3 times more likely to have uncontrolled asthma compared to those attending Khartoum North hospital (OR = 2.96 [1.27–6.86]). Although both hospitals are tertiary, however, this could be explained by that the latter has a specialized asthma emergency room. In Nigeria, as of many LMICs, health-service factors such as poor awareness and knowledge among physicians regarding asthma guidelines, suboptimal infrastructure and diagnostic facilities, and non-availability and high cost of asthma medications were associated with poor asthma control.[10,27] In fact, we found that the use of diagnostic tools for asthma diagnosis and management was very low since only 15.7% of patients had undergone peak flow meter measurement and only 12.4% were diagnosed for asthma using spirometry. Lung function assessment is recommended in asthma care and underuse of these tools has been associated with undertreatment of asthma and poor asthma control.[28]
Longer time to reach health facility was associated with asthma control in this study. This is likely to lead to infrequent follow-up care for asthma as patients are likely to attend only when they have severe symptoms.[20] Previous studies have also reported that underuse and access to healthcare are associated with poorer asthma control.[29]
Family history of asthma is a known risk factor for asthma;[30] however, its association with asthma control is not known; some reported that family history of asthma is not a key factor in asthma control once the guidelines are followed.[31] We found that a family history of asthma is significantly associated with uncontrolled asthma. This might be due to those who had a family history of asthma may have better asthma control knowledge.
In this study, uncontrolled asthma was associated with oral steroids use without prescription (OR = 9.01 [1.01–79.88]). This is similar to findings from another study where uncontrolled asthma was significantly associated with oral steroid dispensing (OR = 2.6 [1.9–3.5]) even after adjusting for demographic characteristics.[32] The use of oral steroids without prescription might indicate that these patients were not on regular controller medication or with a more severe form of disease and therefore they were experiencing asthma control difficulties.
We also found in this study, non-adherence to follow-up is associated with uncontrolled asthma. Similarly, in the Maghreb, asthma control was associated with the frequency of physician consultation, with subjects who consulted less frequently for asthma being better controlled. This reflected the fact that the majority of study subjects only consulted their physician in case of exacerbations, with only one-third of them reporting programmed follow-up consultations.[24]
Inhaler technique was associated with asthma control in this study. This finding is consistent with reports from several studies. A study conducted in Saudi Arabia revealed that improper use of asthma inhaler was associated with uncontrolled asthma.[11] Similarly, reports from Ethiopia[25] and Nigeria[33] showed that incorrect inhaler technique was associated with uncontrolled asthma with an OR of 2.5 (1.26–4.98) and 18.9 (2.3–155.6), respectively. Improper use of inhalers might possibly lead to a reduction in drug delivery and drug effectiveness and consequently contributes to uncontrolled asthma found among these patients.
One of the strengths of our study is that this is the first report of the level of asthma control and its associated factors from Sudan, adding data to the wider MENA region. The cross-sectional nature of the study brings with it its limitation, including that the associations do not imply causality. As patients were selected on the basis of self-report, this may have resulted in selection bias. Moreover, patients were recruited from outpatient’s clinics and this may have increased the prevalence of uncontrolled asthma reported in this study. Recall bias may have also influenced the responses provided by the patients with uncontrolled asthma compared to those with controlled asthma to some events such as their adherence to follow-up visits and steroids tablets use. Moreover, the number of participants with controlled asthma was small and made some associations difficult to establish or to interpret. Although we have recruited patients from all over Khartoum state, exclusion of the other healthcare facilities, including the private and military hospitals, would limit the generalizability of the results. Nevertheless, the study has the merit of reporting the level of asthma control and its associated factors among Sudanese patients attending tertiary care hospitals. These findings, coupled with further research including different care levels, will enable tailoring targeted management interventions.
CONCLUSION
The level of asthma control reported in this study is very low despite the possibility of applying proven, cost-effective interventions in LMICs, particularly asthma SCM.[6,34,35] Our study adds important new data on the factors associated with asthma control among Sudanese patients attending these tertiary care hospitals. Our finding highlights the need for an integrated approach to asthma management where patient’s knowledge about asthma control, including the need for adherence to medication, adherence to follow-up visits, and inhaler technique training, is prioritized.
Acknowledgments
We thank the Pan African Thoracic Society Methods for Epidemiologic, Clinical, and Operations Research (PATS-MECOR) faculty staff for their contribution during the preparation of the study protocol and professor of community medicine Daffalla AlamAlhuda for reviewing the manuscript. We also thank all the participants and the staff at Ibrahim Malik, Khartoum North, and Omdurman Teaching Hospitals for making this survey possible.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet Respir Med. 2017;5:691-706.
- [Google Scholar]
- Prevalence of symptoms of asthma, rhinitis and eczema in 13-to 14-year-old children in Africa: The international study of asthma and allergies in childhood phase III. Allergy. 2007;62:247-58.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and risk factors of asthma symptoms in adult Sudanese using a modified ISAAC questionnaire. Int J Sci Res. 2016;5:1153-6.
- [CrossRef] [Google Scholar]
- The Global Asthma Report 2018 Auckland, New Zealand: Global Asthma Network; 2018. Available from: http://www.globalasthmareport.org [Last accessed on 2020 Feb 06]
- [Google Scholar]
- Sudan Federal Ministry of Health. Annual Health Statistical Report 2017. Available from: http://www.sho.gov.sd/controller/knowledge_hub.php?mid=110&sm_id=132&lid=1 [Last accessed on 2020 Feb 07]
- [Google Scholar]
- Standard case management of asthma in Sudan: A pilot project. Public Health Action. 2013;3:247-52.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Asthma: A Guide to the Essentials of Good Clinical Practice Paris, France: International Union Against Tuberculosis and Lung Disease; 2008.
- [Google Scholar]
- Achieving asthma control in practice: Understanding the reasons for poor control. Respir Med. 2008;102:1681-93.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and practice assessment, and self reported barriers to guideline based asthma management among doctors in Nigeria. Niger J Clin Pract. 2019;22:692-700.
- [Google Scholar]
- Asthma in Nigeria: Are the facilities and resources available to support internationally endorsed standards of care? Health Policy. 2011;99:250-4.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with poor asthma control in the outpatient clinic setting. Ann Thorac Med. 2015;10:100.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with asthma control among adults in five New England states, 2006-2007. J Asthma. 2011;48:581-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adequacy of asthma management among patients attending referred clinics in Khartoum. Khartoum Med J. 2011;4:532-8.
- [Google Scholar]
- Development of the asthma control test: A survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59-65.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of the Arabic version of the asthma control test. Ann Thorac Med. 2008;3:44-7.
- [CrossRef] [PubMed] [Google Scholar]
- Repeated cross-sectional survey of patient-reported asthma control in Europe in the past 5 years. Eur Respir Rev. 2012;21:66-74.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of uncontrolled asthma in adult and pediatric patients: Analysis of the asthma control characteristics and prevalence survey studies (ACCESS) J Asthma. 2010;47:257-62.
- [CrossRef] [PubMed] [Google Scholar]
- Level of asthma control and healthcare utilization in Latin America. Allergy. 2013;68:1463-6.
- [CrossRef] [PubMed] [Google Scholar]
- Level of asthma control and health care utilization in Asia-Pacific countries. Respir Med. 2014;108:271-7.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma management and control in Nigeria: The asthma insight and reality Nigeria (AIRNIG) study. Expert Rev Respir Med. 2019;13:917-27.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma control in adults in the Middle East and North Africa: Results from the ESMAA study. Respir Med. 2018;138:64-73.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of asthma control using asthma control test in chest clinics in Cameroon: A cross-sectional study. Pan Afr Med J. 2016;23:70.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with uncontrolled asthma in adult asthmatics in Kinshasa, democratic republic of congo. PLoS One. 2019;14:e0215530.
- [CrossRef] [PubMed] [Google Scholar]
- Control of asthma in the Maghreb: Results of the AIRMAG study. Respir Med. 2009;103(Suppl 2):S12-20.
- [CrossRef] [Google Scholar]
- Level of asthma control and risk factors for poor asthma control among clinic patients seen at a Referral Hospital in Addis Ababa, Ethiopia. BMC Res Notes. 2017;10:558.
- [CrossRef] [PubMed] [Google Scholar]
- Global Strategy for Asthma Management and Prevention. 2019. Available from: http://www.ginasthma.org [Last accessed on 2020 Mar 23]
- [Google Scholar]
- Nationwide survey of the availability and affordability of asthma and COPD medicines in Nigeria. Trop Med Int Health. 2020;26:54-65.
- [CrossRef] [PubMed] [Google Scholar]
- The use of spirometers and peak flow meters in the diagnosis and management of asthma among Spanish pediatricians. Results from the TRAP study. Pediatr Allergy Immunol. 2004;15:365-71.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of asthma control in a random sample of asthmatic patients. J Asthma. 2007;44:341-5.
- [CrossRef] [PubMed] [Google Scholar]
- The association between family history of asthma and the prevalence of asthma among US adults: National health and nutrition examination survey, 1999-2004. Genet Med. 2009;11:323-8.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of genetic factors (family history of asthma) on long-term asthma control in children. Chest. 2018;154:806A.
- [CrossRef] [Google Scholar]
- Reliability and predictive validity of the asthma control test administered by telephone calls using speech recognition technology. J Allergy Clin Immunol. 2007;119:336-43.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma control among patients in Uyo South-Eastern Nigeria. Indian J Allergy Asth Immunol. 2013;27:27.
- [CrossRef] [Google Scholar]
- Management of asthma in Benin: The challenge of loss to follow-up. Public Health Action. 2013;3:76-80.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma as a hidden disease in rural China: Opportunities and challenges of standard case management. Public Health Action. 2012;2:87-91.
- [CrossRef] [PubMed] [Google Scholar]






