Translate this page into:
Pseudotumoral pulmonary tuberculosis secondary to a paradoxical reaction in an immunocompetent patient from Benin: A case report
*Corresponding author: Attannon Arnauld Fiogbe, Department of Pulmonology Service, National University Hospital of Respiratory Diseases and Tuberculosis, Cotonou, Benin. afiogbe@yahoo.fr
-
Received: ,
Accepted: ,
How to cite this article: Fiogbe AA, Wachinou AP, Ewedje R, Agodokpessi G. Pseudotumoral pulmonary tuberculosis secondary to a paradoxical reaction in an immunocompetent patient from Benin: A case report. J Pan Afr Thorac Soc 2023;4(1): 46-9.
Abstract
Paradoxical reactions (PR) during tuberculosis treatment are rare in HIV negative subjects and result in polymorphic clinical presentations which could sometimes lead to confusion. We report the case of a postpartum mother, HIV negative who was placed on treatment for pulmonary tuberculosis. She experienced transient clinical improvement and developed PR which mimicked lung malignancy. This is a rare phenomenon and may result in diagnostic and therapeutic dilemma in resource poor settings.
Keywords
Pseudotumoral tuberculosis
Paradoxical reaction
Benin
INTRODUCTION
Paradoxical reaction (PR) is an increase in severity of pre-existing lesions or the occurrence of new tuberculous lesions following initiation of an effective anti-tuberculosis (TB) treatment. It is made when medication adherence is assured with secondary deterioration in the patient’s clinical condition.[1-3] It is well known in persons infected with HIV,[1] but could occur in HIV negative persons. Clinical manifestations of non-HIV PR are comparable to those associated with HIV and include, lymphadenopathy with the central nervous system and the lungs most frequently involved.[2] The radio clinical presentation can be polymorphic and sometimes confusing, especially when atypical forms are encountered. PR that presents as a pseudotumoral lesion simulating lung cancer is rare and could lead to confusion among clinicians, with recourse to several invasive investigations. We report here a case of pseudotumoral TB secondary to a PR to TB treatment. We will discuss based on the literature, the mechanism underlying the occurrence of PR, and the diagnostic difficulties inherent to this case management.
CASE REPORT
This was a 23-year-old, postpartum mother, with a body mass index (BMI) of 17 kg/m2, who had been admitted for mild hemoptysis. Her clinical history includes 14 weeks of evening fever, a chronic cough with mucopurulent sputum and right basithoracic pain of moderate intensity. She was previously admitted at a peripheral health center, where the chest radiography had found a thick-walled right apical excavation [Figure 1a]. Her sputum GeneXpert examinations were negative on two occasions. In view of her clinical and radiographic signs, the diagnosis of pulmonary TB (pTB) was made. She was commenced on standard TB treatment for 6 months according to the national guidelines. She reported a transient improvement in symptoms after 1 month of treatment following which she experienced reoccurrence with resurgence of hemoptysis. This made her to discontinue treatment after 4 weeks. She was referred to the district hospital where she was noted to have alteration with the WHO performance status of 2, no fever, a regular tachycardia at 120 beats/min, a respiratory frequency of 21 cycles/min, and oxygen saturation of 96%. She had a hemoglobin = 12.7 g/d and lymphopenia at 1150/ mm3. HIV and hepatitis serologies were negative. The chest radiography, performed 3 months after the previous one, showed a rounded dense homogeneous opacity located in the upper right lobe [Figure 1b]. Chest computed tomography scan revealed: A right hiloapical heteronodular lesion measuring 7 × 9 cm; with central area of necrosis. There was no mediastinal lymphadenopathy [Figure 2]. Based on the suspicion of a neoplastic lesion, she underwent bronchoscopy with bronchioloalveolar lavage (BAL) of the right upper lobe and biopsy of the spurs. There was no endobronchial mass but there were large purulent secretions in the right upper lobe. The microscopy examination performed on the BAL was negative, but the GeneXpert on the same sample identified the DNA of Mycobacterium tuberculosis. Pathological examination of the bronchial biopsy specimens found a cytohistological lesion suggestive of bronchitis caseoexudative TB [Figure 3: histopathological aspect]. The diagnosis of the right apical pseudotumoral TB was, therefore, confirmed. The patient was recommenced on TB treatment for 6 months, with a good clinical and radiological outcome [Figure 4: end treatment radiography].
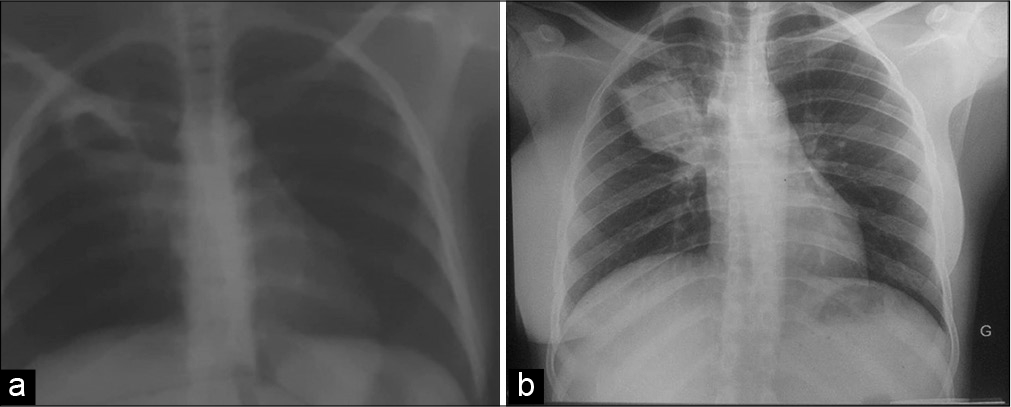
- (a) Chest radiography showing the progression from an excavated lung lesion with thickened walls initially (b) to a pseudo-nodular lung lesion after three months.
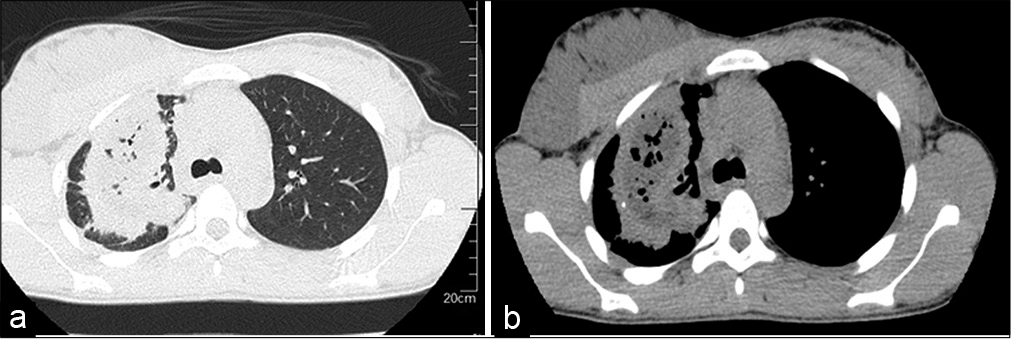
- (a): Transverse parenchymal CT scan showing a spiculated apical mass with areas of necrosis. (b) Mediastinal CT scan showing a right apical heteronodular lesion; multi-cavity with central necrosis.
![Cyto-histological appearance suggestive of caseous-exudative tuberculous bronchitis (zoom x 10) [A]: gigantocellular epithelioid granuloma [B]: zone of caseous necrosis [C]: bronchial glands](/content/124/2023/4/1/img/JPATS-4-046-g003.png)
- Cyto-histological appearance suggestive of caseous-exudative tuberculous bronchitis (zoom x 10) [A]: gigantocellular epithelioid granuloma [B]: zone of caseous necrosis [C]: bronchial glands
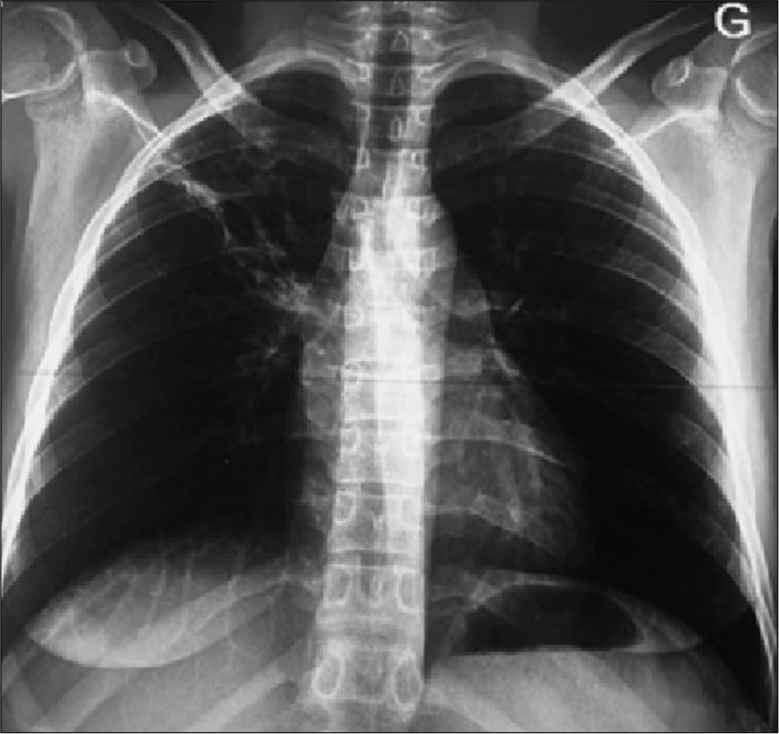
- Chest x-ray at the end of treatment showing complete regression of the right apical lesion after 6 months of complete treatment.
DISCUSSION
pTB remains a major public health problem. The pseudotumoral form is a diagnostic dilemma and that requires invasive procedures that could lead to diagnostic delay. According to Daoudi et al.,[3] in addition to bronchoscopy, it may be necessary to perform ultrasound-guided transthoracic biopsy for pathological examination for the diagnosis.
PR giving a pseudotumoral lesion simulating lung cancer is rare. In 2019, five cases of new pulmonary masses were found by CT scans during the follow-up of patients treated for TB resulting from PR.[4] This clinical presentation is also rare in Benin. To the best of our knowledge, we are presenting the first case of PR giving a pseudotumoral lesion in the nation, after the case of endobronchial TB simulating a cancer published in 2009 by Agodokpessi et al.[5]
One of the clinical particularities of this case is the progressive evolution of a cavitary lesion with a thickened wall into a mass with spiculated margins, few weeks after TB treatment initiation, after a transient clinical improvement. This clinical and especially radiological evolution was suggestive of a PR. Known to often lead to secondary occurrence of extrathoracic TB (lymph nodes, pleurisy, meningitis, or bone), a few case series of pseudotumoral lesion have been reported.[3]
PR occurs when there is a high levels of inflammatory reaction associated with a strong inflammation of the TH1 type.[6] This reaction actually implies a reversion of immunosuppression induced by M. tuberculosis, associated with an exacerbated and deleterious pro-inflammatory profile caused by the efficacy of the treatment.[7] Indeed, the monitoring of the inflammatory profile during the treatment shows an increase in pro-inflammatory cytokines, in particular TNF, and a decrease in anti-inflammatory cytokines such as IL-10, thus restoring the immune balance.[8] In this case report, it is probable that the restoration of immunity led to an uncontrolled inflammatory reaction, which resulted in the formation of an exuberant granulomatous lesion giving the change to a tumor like mass.
Extra-thoracic locations, especially lymph nodes and the brain, malnutrition, and initial lymphopenia are the principal risk factors for PR in TB.[7] Some of these risk factors were found in this patient including low BMI and lymphopenia and especially the postpartum period. The postpartum period, due to a recovery of immunity, would be a favorable period for the occurrence of PR.[9] In pregnant women, the rigorous immunotolerance during gestation stops after childbirth, with an inflammatory profile of the TH1 type,[10] therefore predisposing to a possible runaway inflammatory response.
One of the characteristics of TB pseudotumors is the negativity of microscopy which is related to the poor oxygenation of the caseous lesions.[11] For this patient, we needed BAL to confirm the diagnosis of TB by GeneXpert test which delayed the diagnosis. The temporal profile for PR in TB is usually within 40 ± 20 days as was found in this patient.[7]
CONCLUSION
The occurrence of a PR leading to the change with a pseudotumoral mass is rare. It is usually a diagnostic challenge especially in the context of resource limited countries, where facilities are not readily available in many hospital settings. PR should be considered in at risk patients with worsening symptoms or recurrence of symptoms after a period of some improvement on TB treatment.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Paradoxical reactions during tuberculosis treatment in patients with and without HIV co-infection. Thorax. 2004;59:704-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002;21:803-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pseudotumoral bronchopulmonary tuberculosis mimicking cancer in an immunocompetent patient. Pan Afr Med J. 2019;32:170.
- [CrossRef] [Google Scholar]
- Paradoxical reaction in the form of new pulmonary mass during anti-tuberculosis treatment: A case series and literature review. Infect Drug Resist. 2019;12:3677-85.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculose endobronchique simulant un cancer bronchique. J Afr Thorax Vaisseaux. 2013;3:238-42.
- [Google Scholar]
- Increased levels of circulating interleukin-18 in patients with advanced tuberculosis. Am J Respir Crit Care Med. 2000;161:1786-9.
- [CrossRef] [PubMed] [Google Scholar]
- Paradoxical reaction following tuberculosis treatment in non HIV-infected patients. Rev Mal Respir. 2020;37:399-411.
- [CrossRef] [PubMed] [Google Scholar]
- Cytokines and acute phase serum proteins as markers of inflammatory regression during the treatment of pulmonary tuberculosis. J Bras Pneumol. 2008;34:942-9.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated tuberculosis after pregnancy progressed to paradoxical response to the treatment: report of two cases. BMC Infect Dis. 2016;16:284.
- [CrossRef] [PubMed] [Google Scholar]
- IL-12, TNF-alpha, and hormonal changes during late pregnancy and early postpartum: Implications for autoimmune disease activity during these times. J Clin Endocrinol Metab. 2001;86:4933-8.
- [CrossRef] [PubMed] [Google Scholar]







