Translate this page into:
Value of Adenosine Deaminase in the diagnosis of tuberculous pleurisy at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia
*Corresponding author: Amsalu Bekele Binegdie, Department of Internal Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia. amsalubekele2016@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Binegdie AB, Ashagire AW, Brandli O, Sherman C, Schluger NW, Schoch O. Value of Adenosine Deaminase in the diagnosis of tuberculous pleurisy at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. J Pan Afr Thorac Soc 2022;3:65-70.
Abstract
Objectives:
Tuberculous (TB) pleurisy is a common form of extrapulmonary tuberculosis in high burden countries including Ethiopia. Adenosine deaminase (ADA) has been used in the early diagnosis of TB pleurisy. This study was designed to evaluate the diagnostic role of ADA in TB pleurisy at Tikur Anbessa Specialized Hospital (TASH).
Materials and Methods:
A cross-sectional hospital-based study was designed to evaluate the diagnostic value of ADA in consecutive adult patients with unexplained pleural effusions presenting to Chest Clinic at TASH from June 2016 to August 2018. All referred patients underwent thorough clinical and laboratory examinations including assessment of pleural fluid ADA, where a value of ≥40 IU/I was used to suggest TB pleurisy (per manufacturer’s recommendation). A final diagnosis of TB pleurisy was made based on pleural fluid Gene Xpert, AFB smear, pleural biopsy, and cytology results in addition to a clinical and radiologic response to anti-TB therapy.
Results:
A total of 67 patients were included in the study. The median age was 38.5(±14.5) years; 36 (53.7%) of the participants were males. TB pleurisy was confirmed in 38 (56.7%) subjects. The mean pleural fluid ADA levels was significantly higher in those with TB pleurisy as compared to those without TB pleurisy, 65.8 IU/l versus 28 IU/I (P < 0.05), respectively. Pleural fluid ADA had a sensitivity of 84% and specificity of 79%, resulting in a positive predictive value of 84.2%, a negative predictive value of 79.3%, and an overall test accuracy of 82% in our study population.
Conclusion:
In our study, pleural fluid ADA played a useful role in the diagnosis of TB pleurisy.
Keywords
Adenosine deaminase
Pleurisy
Tuberculosis
INTRODUCTION
Tuberculous (TB) pleurisy is a one of the most common manifestations of extra-pulmonary tuberculosis and the main cause of pleural effusions in many high TB burden countries.[1,2] The clinical and economic cost of a delayed diagnosis of TB pleurisy can be significant, especially in low- and middle-income countries.
According to 2020 Global TB Report, Ethiopia is one of the highest TB and TB/HIV affected countries in the world, with an annual estimated TB incidence of 140/100,000 population and a death rate of 19/100,000 populations.[3] Further, Ethiopia is the third highest country affected by extrapulmonary TB (EPTB) with TB pleurisy occurring in 13.5% of EPTB cases.[4,5]
The diagnosis of TB pleurisy remains challenging because of the low sensitivity of various traditional investigations. Lymphocytic exudates, found in TB pleural effusion, can also occur in other diseases such as malignancy and collagen vascular diseases such as rheumatoid arthritis and systemic lupus erythematous.[6-8] Cultures for acid-fast bacilli are positive in only 20–30% of pleural fluid specimens and in 50–80% of pleural biopsies.[9,10]
More recently, early diagnosis of TB pleurisy has greatly improved using nucleic acid amplification and biochemical markers such as adenosine deaminase (ADA), interferon-gamma, and lysozyme.[6,11-18] Each of these tests has strengths and weaknesses, although ADA offers the most promise for widespread usage.
ADA, an enzyme produced from lymphocytes, has been extensively studied in TB pleurisy. The ADA assay is a simple, rapid, relatively inexpensive, and minimally invasive test that can be performed in most laboratories.[2] ADA elevation in tuberculosis pleural effusion has been reported to have a sensitivity and specificity of 91–100% and 81–94%, respectively.[6,16,19,20] In addition, the positive and negative predictive values for ADA in TB pleurisy range from 84% to 93% and 89% to 100%, respectively.[6,16,19,20]
The diagnostic performance of the ADA assay for TB pleurisy has not been studied in Ethiopia, one of the high TB burden countries in the world. The purpose of this research was to assess the sensitivity, specificity, positive, and negative predictive values of ADA in the diagnosis of TB pleurisy at Tikur Anbessa Specialized Hospital (TASH), the largest public hospital in Addis Ababa, Ethiopia.
MATERIALS AND METHODS:
A cross-sectional, hospital-based study was conducted from June 2016 to August 2018 to investigate the utility of pleural fluid ADA in the diagnosis of TB pleurisy. The study population comprised all consecutive patients, ≥18 years of age, referred to Chest Clinic at TASH, Addis Ababa, Ethiopia for evaluation of unexplained pleural effusions after initial investigations.
Each patient underwent a comprehensive clinical history and physical examination. In addition, repeat thoracentesis was performed and the pleural fluid sent for ADA, Gene Xpert-MTB/RIF (Gene Xpert), based on availability, and acid-fast bacilli (AFB) smear (both pleural and sputum specimens), when possible, biochemistry (glucose, protein, and LDH), and cytology. Chest X-rays were obtained on all participants and pleural biopsy was performed on a subset of the study group. Serum for rheumatoid factor (RF) and anti-nuclear antibodies (ANA) was also obtained to evaluate for connective tissue disease.
Light’s criteria were used to categorize the pleural effusions as exudative or transudative in character.[21]
Patients with pleural fluid ADA ≥40 IU/l, the manufacturer’s cutoff highly suggestive of TB pleurisy, and those with other diagnostic tests consistent with TB pleurisy were treated with 6 months of standard anti-TB therapy. Treatment response, using clinical improvement in respiratory symptoms and weight gain in addition to radiographic resolution of pleural fluid, was determined at the 2nd, 5th, and 6th months of treatment.
TB pleurisy was confirmed by the results of diagnostic investigations and/or full clinical recovery and complete resolution of the pleural effusions on anti-TB treatment.
ADA kits (Diazyme Europe GmbH) were donated by the Swiss Lung Foundation (Zurich, Switzerland) through East African Training Initiatives and appropriately stored and utilized following the manufacturer’s instructions.
Data analysis
Data were analyzed using SPSS (version 21.0) statistical software. The mean ± standard deviation and proportions were calculated for continuous and categorical data, respectively. Median and interquartile range (IQR) were used for non-normally distributed numerical data. The Student’s t-test was used to compare means and P < 0.05 was considered significant. Sensitivity, specificity, and positive and negative predicted values were calculated using standard definitions. Odds ratio (OR) estimates and 95% confidence intervals (CI) were calculated to evaluate associations between TB pleurisy and age, gender, residence, HIV status, occupation, smoking, and ADA level.
Ethical approval
All participants provided written informed consent. Ethical approval for the study was obtained from the Institutional Review Board of the College of Health Sciences, Addis Ababa University. The study was conducted under principles and guidance of ethical standards.
RESULTS
A total of 67 patients with previously undiagnosed pleural effusions were included in the study, socio-demographics are shown in [Table 1]. A majority of patients were male (n = 36; 53.7%) and most were from urban areas (n = 41; 61%). HIV testing was done for all patients; 5 (7.5%) tested positive.
| n=67 | Character | Total | Confirmed TB Pleurisy | Non-TB Pleurisy | Crude OR with 95% OR (Confidence Interval) |
|---|---|---|---|---|---|
| Total | 67 (100%) | 38 (56.7%) | 29 (43.3%) | ||
| Gender | Male | 36 | 22 | 14 | 1.47 (0.58–1.18) |
| Female | 31 | 16 | 15 | ||
| Age category | |||||
| Q1 | 18–32 | 28 | 16 | 12 | |
| Q2 | 33–46 | 19 | 12 | 7 | 1.93 (1.76–4.72) |
| Q3 | 4–60 | 7 | 3 | 4 | 2.29 (2.62–5.830 |
| Q4 | 60–74 | 13 | 7 | 6 | 1.33 (4.20–8.18) |
| Residency | Urban | 41 | 25 | 16 | 1.56 (0.55–1.26) |
| Rural | 26 | 13 | 13 | ||
| HIV status | Negative | 62 | 34 | 28 | 0.30 (−3.44–0.64) |
| Positive | 5 | 4 | 1 | ||
| Occupation | Gov’t | 28 | 16 | 12 | 0.952 (0.30–1.71) |
| Private | 24 | 14 | 10 | ||
| House wife | 15 | 8 | 7 | ||
| Smoking | No | 61 | 36 | 25 | 2.88 (0.72–2.50) |
| Yes | 6 | 2 | 4 | ||
| ADA value | ≥40 IU/L | 38 (56.7%) | 32 (47.8) | 6 (9%) | - |
| <40 IU/L | 29 (43.3%) | 6 (9.0%) | 23 (34.3%) | 16.8 (4.96–56) |
TB: Tuberculous, ADA: Adenosine deaminase, OR: Odds ratio
The age range of study participants was 18–74 years with a median age of 38.5 years (IQR ± 14.5 years). Age groups of 18–34 years and 35–44 years were most represented, with 28 (41.8%) and 19 (28.4%) participants, respectively.
Using Light’s criteria, almost all subjects (n = 64, 95.5%) had exudative pleural effusions; only 2 had transudates attributed to CHF.
The diagnosis of TB pleurisy was confirmed in 38 (56.7%) patients based on clinical and radiographic response to anti-TB treatment (n = 38) and/or Gene Xpert (n = 8; pleural fluid (2) and sputum (6)), AFB smear (n = 3), pleural biopsy (n = 7), and cytology (n = 20) (proteinaceous background with lymphocyte predominance, no mesothelial cells, and no malignant cells). The remaining 29 (43.3%) of patients had a combination of diseases including 20 (30.0%) malignancy (confirmed by cytology), 6 (9.0%) connective tissue disease (confirmed by serum RF and ANA), and 3 (4.5%) congestive heart failure [Figure 1].
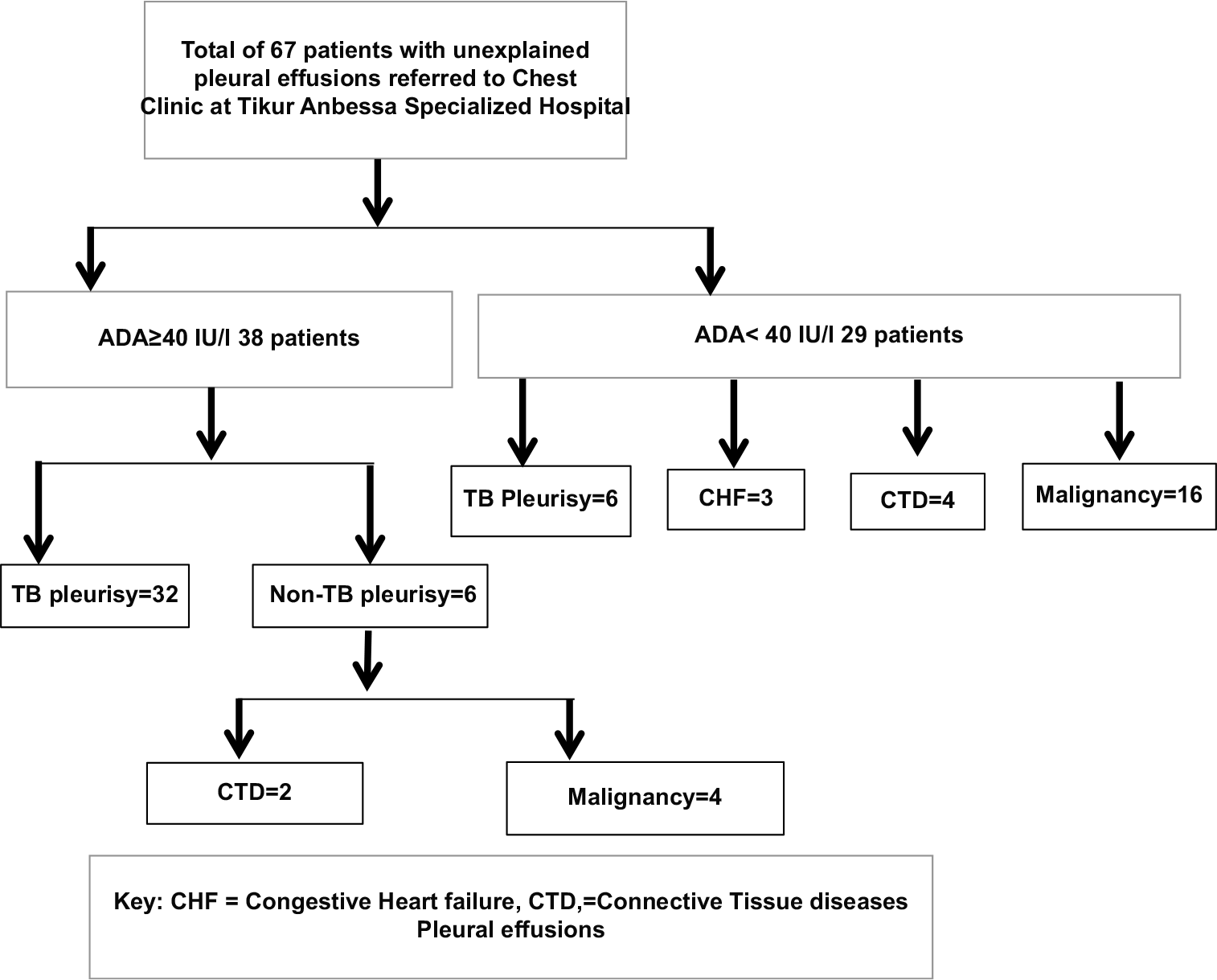
- Study participant flow chart.
The average ADA value for the study participants was 47.5 ± 28.5 IU/l and ranged from 6-110 IU/l. The mean pleural fluid ADA level was significantly higher for patients with TB pleurisy (65.8 ± 25.8 IU/l) than for those without TB pleurisy (28.0 ±10 IU/l) (p<0.05). Only age and ADA values were associated with TB pleurisy [Table 1]. ADA values were ≥40 IU/l in 32 (84.2%) subjects with confirmed TB pleurisy and in 6 (15.8%) of those without TB pleurisy. Conversely, 6 (20.7%) participants with confirmed TB pleurisy and 23 (79.3%) without TB pleurisy had ADA values <40 IU/l [Table 2].
| ADA value | No (%) | Confirmed TB Pleurisy | Non-TB pleurisy | Sensitivity % | Specificity % | PPV % | NPV % |
|---|---|---|---|---|---|---|---|
| ADA<40 IU/l | 29 (43.3) | 6 (9.0) | 23 (34.3) | ||||
| ADA≥40IU/l | 38 (56.7) | 32 (47.8) | 6 (9.0) | ||||
| Total | 67 (100) | 38 (56.7) | 29 (43.3) | 84.2% | 79.3% | 84.2% | 79.3% |
TB: Tuberculous, ADA: Adenosine deaminase, PPV: Positive predictive value, NPP: Negative predictive value
The sensitivity and specificity of ADA in diagnosing TB pleurisy were 84.2% and 75.9%, respectively. The positive and negative predictive values of the test were 82.1% and 78.6%, respectively [Table 2]. The positive and negative likelihood ratios of the test were 4.1 and 0.2, respectively. The test agreed 82.1% of the time with a pre-test probability of 57%.
DISCUSSION
In our study of 67 patients with unexplained pleural effusion, TB pleurisy was confirmed in 38 patients. Pleural fluid ADA levels were useful in differentiating TB pleurisy from other causes of pleural effusions. An ADA cutoff value of 40 IU/l (as recommended by the manufacturer) showed high sensitivity and specificity with high positive and negative predictive values for the diagnosis of TB pleurisy.
Even though our definition of TB pleurisy relied, in part, on a clinical response to TB treatment, our patients were like the general population of TB patients in Ethiopia. We had a predominance of men, reflecting the gender distribution in the country (22). The most commonly affected age group was 18–34 years, followed by those 35–44 years, which is consistent with the national age distribution of TB patients in Ethiopia.[22]
The ADA level in pleural fluid has been used as a strong marker for TB pleurisy with a sensitivity of 81–100% and specificity of 83–100% in other studies.[22-25] The diagnostic value of ADA testing depends on the local prevalence of TB. Two studies from South Africa found sensitivity values of 80–83.6% and specificity values of 83.6–94%.[26,27] Our results are generally consistent with these findings from another high TB burden country.
Measuring ADA isoenzyme levels can improve the diagnostic accuracy of ADA for TB pleurisy.[19] ADA-2 isoenzyme increases in patients with TB effusions, whereas ADA-1 isoenzyme is increased in other bacterial causes of pleural disease. In two different studies, measures of ADA-2 isoenzyme increased the specificity for TB pleurisy from 91% to 96% and 92.1% to 98.6%.[20,22,28] In our study, we measured total ADA level in pleural fluid and not specific isoenzymes, which could partially explain our lower sensitivity and specificity.
The utility of ADA in immunocompromised patients has not been well studied. Baba et al. showed that ADA was a consistent marker of pleural TB in HIV-positive patients, regardless of CD4 counts.[29] Chung et al. found similar findings in renal transplant recipients.[30] In our study, 4 of the 5 HIV-positive patients were in the TB pleurisy group and had elevated ADA levels.
Limitations of the study
There were several study limitations. Our study sample size was small which may have influenced our results. Patients were recruited from a tertiary referral hospital which may limit the generalizability of our results. As previously mentioned, ADA levels were quantitatively measured without analysis of isoenzyme types. Finally, our definition of TB pleurisy may have influenced our results.
CONCLUSION
Our study findings indicate that ADA level is potentially used diagnostic tool for TB pleurisy in Ethiopia, and likely other low- and middle-income countries. Future prospective studies are needed to confirm our findings before large-scale programmatic changes can be recommended in high burden countries.
Acknowledgments
I would like to thank the dedicated laboratory technicians who performed the ADA test for the study participants and the nurses and resident physicians working in the Chest Unit of TASH who recruited study participants. In addition, I would like to thank the Swiss Lung Foundation (Zurich, Switzerland) for providing funding and technical expertise.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This study was supported by The Swiss Lung Foundation, Switzerland.
Conflicts of interest
There are no conflicts of interest.
References
- Update on tuberculous pleural effusion. Respirology. 2010;15:451-8.
- [CrossRef] [PubMed] [Google Scholar]
- Global Tuberculosis Report. 2020. Geneva: World Health Organization; Available from: https://www.who.int/tb/global-report-2020
- [Google Scholar]
- Clinical, molecular, and drug sensitivity pattern of mycobacterial isolates from extra-pulmonary tuberculosis cases in Addis Ababa, Ethiopia. BMC Infect Dis. 2015;15:456.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and the diagnostic challenge of extra-pulmonary tuberculosis in a teaching hospital in Ethiopia. PLoS One. 2020;15:e0243945.
- [CrossRef] [PubMed] [Google Scholar]
- Pleural biopsy and adenosine deaminase enzyme activity in effusions of different. Lung India. 1989;7:122-4.
- [Google Scholar]
- Pleural fluid adenosine deaminase in rheumatoid arthritis and systemic lupus erythematosus. Chest. 1984;86:273-4.
- [CrossRef] [Google Scholar]
- Pleural fluid adenosine deaminase in rheumatoid arthritis and systemic lupus erythematosus. Chest. 1984;86:273-4.
- [CrossRef] [Google Scholar]
- Diagnostic procedures for pleural disease. Clin Chest Med. 1985;6:33-48.
- [CrossRef] [Google Scholar]
- Tuberculous pleurisy: An update. Tuberc Respir Dis. 2014;76:153-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of real-time PCR of patient pleural effusion for diagnosis of tuberculosis. BMC Res Notes. 2011;4:279.
- [CrossRef] [PubMed] [Google Scholar]
- Xpert MTB/RIF assay for diagnosis of pleural tuberculosis. J Clin Microbiol. 2011;49:4341-2.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic value of adenosine deaminase in tuberculous pleural effusion: A meta-analysis. Ann Clin Biochem. 2003;40:374-81.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculous pleurisy: A study of 254 patients. Arch Intern Med. 1998;158:2017-21.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of tuberculous pleurisy using the biologic parameters adenosine deaminase, lysozyme, and interferon gamma. Chest. 1993;103:458-65.
- [CrossRef] [PubMed] [Google Scholar]
- Significance of adenosine deaminase activity and its isoenzymes in tuberculous effusions. Chest. 1994;106:33-7.
- [CrossRef] [PubMed] [Google Scholar]
- Use of adenosine deaminase as a diagnostic tool for tuberculous pleurisy. Thorax. 1995;50:672-4.
- [CrossRef] [PubMed] [Google Scholar]
- Value of adenosine deaminase in the diagnosis of tuberculous pleural effusions in young patients in a region of high prevalence of tuberculosis. Thorax. 1995;50:600-3.
- [CrossRef] [PubMed] [Google Scholar]
- Combined use of pleural adenosine deaminase with lymphocyte/neutrophil ratio. Increased specificity for the diagnosis of tuberculous pleuritis. Chest. 1996;109:414-9.
- [CrossRef] [PubMed] [Google Scholar]
- Serum adenosine deaminase: Isoenzymes and diagnostic application. Clin Chem. 1992;38:1322-6.
- [CrossRef] [PubMed] [Google Scholar]
- Adenosine deaminase in the diagnosis of tuberculous pleural effusion: Is it really an ideal test? A word of caution. Chest. 2005;127:417-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adenosine deaminase in the diagnosis of tuberculous pleural effusion. Chest. 2001;120:334-6.
- [CrossRef] [PubMed] [Google Scholar]
- High pleural fluid adenosine deaminase levels: A valuable tool for rapid diagnosis of pleural TB in a middle-income country with a high TB/HIV burden. S Afr Med J. 2014;104:200-3.
- [CrossRef] [PubMed] [Google Scholar]
- The use of real-time polymerase chain reaction and an adenosine deaminase assay for diagnosing pleural tuberculosis. Afr J Lab Med. 2019;8:731.
- [CrossRef] [PubMed] [Google Scholar]
- Serum and pleural adenosine deaminase. Correlation with lymphocytic populations. Chest. 1990;97:605-10.
- [CrossRef] [PubMed] [Google Scholar]
- Adenosine deaminase activity is a sensitive marker for the diagnosis of tuberculous pleuritis in patients with very low CD4 counts. PLoS One. 2008;3:e2788.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnostic value of the adenosine deaminase activity in the pleural fluid of renal transplant patients with tuberculous pleural effusion. Yonsei Med J. 2004;45:661-4.
- [CrossRef] [PubMed] [Google Scholar]






