Translate this page into:
Pleurisy and bilateral pleural effusions after administration of atorvastatin
*Corresponding author: Amsalu Bekele Binegdie, Department of Internal Medicine, College of Health Sciences, Addis Ababa University, Bole, Addis Ababa, Ethiopia. amsalubekele2016@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Binegdie AB, Sherman CB, Schluger NW. Pleurisy and bilateral pleural effusions after administration of atorvastatin. J Pan Afr Thoracic Soc 2020;1(1):39-41.
Abstract
Atorvastatin is a widely used cholesterol-lowering agent. Although generally safe and well tolerated, a number of drug side effects have been reported. We report only the second case of atorvastatin-induced pleural effusions, presenting as pleurisy, and the first case from Ethiopia. We believe our patient had this association based on the temporal onset of symptoms, the otherwise negative evaluation, and the resolution of findings once atorvastatin was discontinued. Clinicians need to consider this relationship when evaluating unexplained pleurisy and pleural effusions in patients taking atorvastatin.
Keywords
Atorvastatin
Pleural effusions
Pleurisy
INTRODUCTION
Atorvastatin is a commonly prescribed statin used to lower cholesterol. It works by inhibiting HMGCoA reductase and increasing the expression of low-density lipoprotein (LDL) receptors in the liver. This, in turn, leads to a reduction in LDL serum levels and a significant decrease in cardiovascular mortality.[1-3] The most common side effects of atorvastatin include muscle pain, myopathy, rhabdomyolysis, and elevations of hepatic enzyme.[4-6] We report only the second case of atorvastatin-induced pleural effusions, presenting as pleurisy, and the first case from Ethiopia. Informed written consent was taken from the patient to use the clinical data for this case presentation.
CASE REPORT
A 68-year-old healthy male visited his primary care physician for a routine office visit. He had no history of hypertension, diabetes, or tobacco use. His physical examination and baseline laboratories including renal and liver function were all normal. His lipid profile showed the following: Serum cholesterol: 167 mg/dl (<200 mg/dl), HDL: 43 mg/dl (>60 mg/dl), and LDL: 118 mg/dl (<130 mg/dl). Despite these results, he was started on atorvastatin 40 mg once daily.
Two weeks after initiation of treatment, he developed left-sided and then subsequent right-sided pleuritic chest pain. He had no fever, chills, pharyngitis, rhinorrhea, cough, or dyspnea. He returned to his primary care physician who obtained a normal CBC; a CXR at the time showed a moderate sized left-sided pleural effusion [Figure 1].
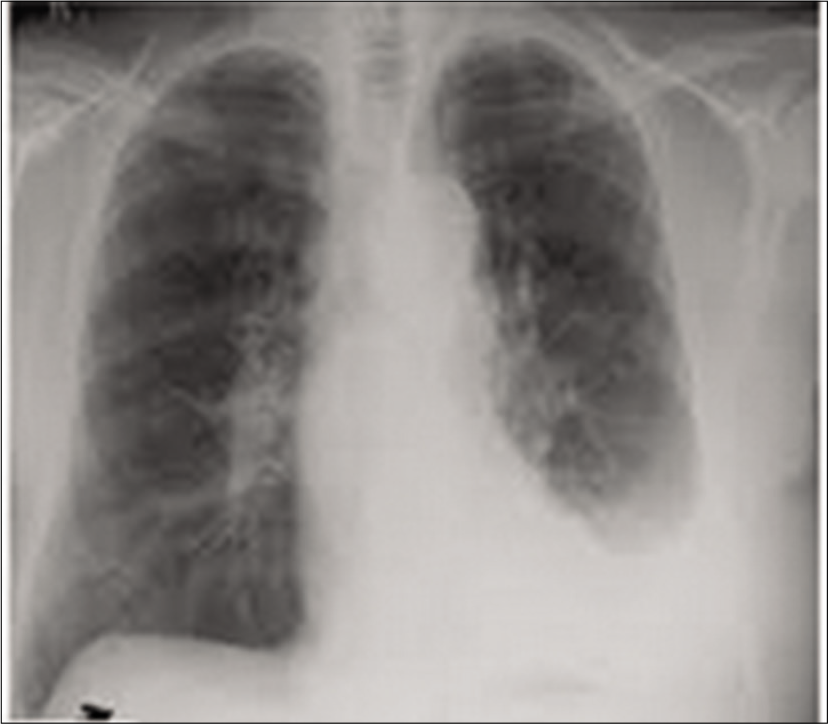
- CXR imaging showed a moderate left-sided pleural effusion.
The patient was then referred to a pulmonologist for further evaluation. A chest CT was obtained and revealed bilateral pleural effusions, left greater than right, with no other abnormalities.
Other laboratory investigations included a normal echocardiogram and negative ANA and RF. Left-sided thoracentesis was performed and the pleural fluid was found to be a lymphocytic transudate with negative cytology, Gram stain, and GeneXpert testing.
Despite the above investigations, the exact cause of the pleural effusions was not identified. The possibility of atorvastatin-induced pleurisy/pleural effusions was considered and the drug was discontinued. His bilateral pleuritic chest pain subsided after 1 week and a repeat CXR 1 month later showed significantly reductions in the bilateral pleural effusions. After 3 months, repeat CXR and chest ultrasound were both normal [Figure 2].

- CXR after 3 months of discontinuation of atorvastatin.
DISCUSSION
We report only the second case of atorvastatin-induced pleural effusions, presenting as pleurisy,[7] and the first case from Ethiopia. We believe our patient had this association based on the temporal onset of symptoms, the otherwise negative evaluation, and the resolution of findings once atorvastatin was discontinued.
In general, drug-induced pleural reactions may occur in the absence of parenchymal lung disease and usually manifest as pleurisy and pleural effusions. The pathologic mechanism remains unknown, but hypersensitivity, oxidative stress of the mesothelial cells, fluid retention, and chemical inflammation have all been postulated.[8,9] To make the diagnosis, clinicians should meticulously review medication use and inquire about a temporal relationship between drug exposure and symptoms. Resolution of symptoms after drug discontinuation, reappearance after drug reuse, and evidence of pleural fluid eosinophilia help to confirm the diagnosis.[6] Treatment is two-fold: Drainage of the pleural fluid to relieve dyspnea and discontinuation of the offending drug. Rarely, corticosteroid administration is required.
CONCLUSION
Clinicians need to consider the relationship between atorvastatin and pleural effusions, presenting as pleurisy, when evaluating patients with unexplained pleural disease.
ACKNOWLEDGMENTS
The authors would like to thank the East African Training Initiative (eatiethiopia.org), Addis Ababa University, Addis Ababa, Ethiopia, Vital Strategies, New York City, New York, USA, and the Swiss Lung Foundation, Zurich, Switzerland, for their support.
We thank the NIHR Global Health Research Unit on Lung Health and TB in Africa at LSTM – “IMPALA” for helping to make this work possible. In relation to IMPALA (grant number 16/136/35) specifically: IMPALA was commissioned by the National Institute of Health Research using Official Development Assistance funding. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Simvastatin-induced pleuro-pericardial effusion and megaloblastic anemia. J Gen Pract. 2015;3:198.
- [CrossRef] [Google Scholar]
- Cholesterol lowering with statin drugs, risk of stroke, and total mortality. An overview of randomized trials. JAMA. 1997;278:313-21.
- [CrossRef] [PubMed] [Google Scholar]
- Discovery, biochemistry and biology of lovastatin. Am J Cardiol. 1988;62:J10-5.
- [CrossRef] [Google Scholar]
- Polymyalgia, hypersensitivity pneumonitis and other reactions in patients receiving HMG-CoA reductase inhibitors: A report of ten cases. Chest. 1999;115:886-9.
- [CrossRef] [PubMed] [Google Scholar]
- Statin-induced fibrotic nonspecific interstitial pneumonia. Eur Respir J. 2002;19:577-80.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral pleural effusions associated with pravastatin sodium treatment. Eur Respir J. 2007;30:1022.
- [CrossRef] [PubMed] [Google Scholar]
- Pleurisy induced by atorvastatin. Rev Mal Respir. 2016;33:607-11.
- [CrossRef] [PubMed] [Google Scholar]






