Translate this page into:
Malignant pleural mesothelioma: A scourge of a disease – An audit of a single South African tertiary center
*Corresponding author: Risenga Frank Chauke, Department of Cardiothoracic Surgery, Sefako Makgatho Health Sciences University/Dr George Mukhari Academic Hospital, Ga-Rankuwa, South Africa. chaukerisa@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chauke RF, Kubheka-Chauke ZB. Malignant pleural mesothelioma: A scourge of a disease – An audit of a single South African tertiary center. J Pan Afr Thorac Soc. 2024;5:82-7. doi: 10.25259/JPATS_9_2024
Abstract
Objectives:
The incidence of malignant pleural mesothelioma (MPM) is on the rise worldwide, especially in low- to medium-income countries (LMICs). Diagnosing and treating MPM poses a significant challenge due to its heterogeneity. Exposure to asbestos fibers can be occupational and environmental in LMICs like South Africa (SA). The latter may be compounded by challenges in rehabilitating abandoned mines in SA since the ban on asbestos mining. Environmental exposure enables MPM compensation inequity as it is currently limited to occupational exposure cases, raising moral concerns. The study sought to assess the incidence of MPM at the Dr George Mukhari Academic Hospital thoracic unit.
Materials and Methods:
A retrospective cross-sectional data analysis involved reviewing data of patients diagnosed with some tumor from all histology specimens collected from pleural biopsies, decortications, pulmonary resections, and lung biopsies from between 2012 and 2021. The data were retrieved from the National Health Laboratory Services database.
Results:
Of the 91 cases diagnosed with some tumor, 34.07% (n = 31) were diagnosed with adenocarcinoma, which was the highest, followed by 23.08% (n = 21) diagnosed with MPM, of which 76.19% (n = 16) were male. About 52.38% of MPM cases were linked to decortication compared to 47.62% from pleural biopsies. No MPM was diagnosed from lung biopsy or pulmonary resection. Most cases, 61.9%, involved patients above 55 years (n = 13), between 35 and 55 years at 33, 33% (n = 7), and 4.75% (n = 1) for age below 35.
Conclusion:
MPM is a public health issue affecting more men than women, and it also affects younger people.
Keywords
Malignant mesothelioma
South Africa
Asbestos
Scourge
Justice
Social determinants of health
INTRODUCTION
Malignant pleural mesothelioma (MPM) is not rare and is considered a silent and invisible epidemic.[1] On the contrary, it is on the rise, including the incidence of asbestos-related diseases, thus making it a rising global public health issue.[1-6] Occupational and non-occupational asbestos exposure is the leading cause of MPM, and its incidence is understated globally because some countries do not have specific cancer registries.[5]
Most MPM longitudinal studies were conducted in the United Kingdom (UK) which has been monitoring MPM mortality rates since 1968, and it’s showing an upward trend despite the ban on asbestos mining in 51 countries, including the UK, which showed an increase from 153 in 1969, 2360 in 2010, and 2291 in 2011. Russia, Indonesia, Pakistan, Brazil, and Nigeria had not imposed such bans. Therefore, it is unsurprising for other countries not to have MPM data, skewing the global incident data, which contributes to underestimating the true disease burden.[7] The increase in MPM cases is significantly observed in low-income regions, and the incidence is declining in developed countries like Sweden, following the total ban two to three decades later.[8]
Rising poverty and unemployment levels contribute to continued mining and use of asbestos despite the bans. Russia, Zimbabwe, Brazil, India, China, and Canada continued mining asbestos.[8] Approximately 1300–3000 cases of MPM are diagnosed in the US and UK annually, and attempts to estimate the global burden are ongoing.[9-11] The reporting status of mesothelioma by national income reflects medical resource capacity, explaining the absence of reports from low-income countries.[5] Despite this, there has been an improvement in MPM-related mortality data in recent years, but data quality varies across countries.[5]
The male-to-female ratio for the risk of MPM is 3:1, with the median age at 73. The median survival period is 6–15 months, despite the stage of the disease. Most mortality data are from Europe and America.[4] By applying gender- and age-specific MPM mortality rates to all other countries, the estimated global burden ranges between 36 300 and 38 400 annual deaths.[4]
There are two types of asbestos fibers: (1) Amphibole, with the following subtypes: Amosite, Crocidolite, Anthophyilite, Tremolite, and Actinolite, and (2) Serperntile, with Chrysotile as the only subtype.[2,3] Amphibole exposure leads to MPM and there is still controversy on the causality of MPM from Chrysotile.[2] The ReNam case series revealed that 80.5% of MPM were exposed to asbestos and ionizing radiation, smoking, and genetic predisposition were other identified risk factors.[2,12] Symian virus 40, exposure from contaminated polio vaccine is a controversial risk factor for MPM and is believed to be declining. Several other risk factors include exposure to erionite, a mineral fiber commonly found in the stones used for building houses in some Turkish villages, and High Aspect Ratio Nanoparticles.[2,3,13]
There are three sub-types of MPM, which are (1) epitheloid (epithelial), found in 50% of cases with longer survival rate, compared to (2) biphasic (mixed), and (3) sarcomatous, with poor survival rates.[2,13] MPM is difficult to diagnose and requires an adequate biopsy specimen for histology and relevant clinical, radiologic, and surgical findings.[11] Identifying actionable gene mutations is challenging, and current treatment options are mainly ineffective and becoming increasingly complex.[3]
Non-invasive diagnostic modalities include blood biomarkers in the form of the soluble mesothelin-related peptide, methylation-specific real-time polymerase chain reaction analysis, oligonucleotide array-based (cGH), and micro-RHA; additionally, positron emission tomography scan can be done to confirm the diagnosis.[13]
Invasive modalities include pleural biopsy done through minimal thoracotomy or video-assisted thoracic surgery; the specimen is sent for histology and immunohistochemistry.[13]
Epithelial markers such as monoclonal and polyclonal carcinoembryonic antigen (CEA) and Ber-EP4 assist in excluding mesothelioma from other carcinomas, and mesothelial markers such as cytokeratin 5/6 and calretinin confirm MPM diagnosis.[14]
Historically, there are three modes of treatment (Trimodal), and the first is surgery, which includes extrapleural pneumonectomy, extended pleurectomy decortication, pleurectomy decortication, or partial pleurectomy.[3] The second modality is adjuvant radiation therapy, where intensity-modulated radiation therapy or external beam radiation therapy is given following surgery. The last modality is chemotherapy in the form of intravenous administration of Alimta plus Alkylating agent.[3]
In the mesothelioma and radical surgery (MARS) 1 trial, although heavily criticized, patients who underwent extrapleural pneumonectomy fared worse than patients who underwent extended pleurectomy decortication.[15]
MARS 2 has not shown any benefits of combining surgery with chemotherapy and radiation therapy over no surgery. Patients who did not undergo surgery survived better than those who had surgery.[16]
Future treatment modalities include immune check-point inhibitors and chemoimmunotherapy, the results of which are currently still too early to conclude. Other future options include cellular therapy, molecular stratified therapy, and genomic and epigenomic landscapes.[17]
However, the survival rate after the diagnosis of MPM is dismal, regardless of the stage of the disease or treatment modality undertaken, with an average of 9 months survival after the initial diagnosis.[18]
MATERIALS AND METHODS
Data description and analysis
A retrospective cross-sectional study pleural biopsies, decortications, and pulmonary resections performed between 2012 and 2021 was done by the Department of Cardiothoracic Surgery at the Dr. George Mukhari Academic Hospital/Sefako Makgatho Health Sciences University complex. Ninety one histology samples were analysed [Table 1]. Data were obtained from the National Health Laboratory Services (NHLS). Ethical approval was obtained from the Sefako Makgatho Health Sciences University’s Research and Ethics Committee (SMUREC). The study used STATA version 15.1 (Stata Corporation, College Station, Texas, USA).
| Types of tumors | Type of surgical procedure | ||||
|---|---|---|---|---|---|
| Decortication (%) | Lobectomy/Pneumonectomy (%) | Pleural biopsy (%) | Lung biopsy (%) | Total (%) | |
| Adenocarcinoma | 1 (3.22) | 1 (3.22) | 29 (93.54) | 0 | 31 (34.07) |
| Mesothelioma | 11 (52.38) | 0 | 10 (47.61) | 0 | 21 (23.08) |
| Carcinoma (unspecified) | 0 | 0 | 13 (100) | 0 | 13 (14.29) |
| Squamous carcinoma | 1 (25) | 2 (50) | 1 (25) | 0 | 4 (4.40) |
| Others | 0 | 5 (22.72) | 14 (63.63) | 3 (13.63) | 22 (24.17) |
| Total | 13 (14.2) | 8 (8.8) | 67 (73.6) | 3 (3.3) | 91 (100) |
RESULTS
MPM was the second most diagnosed tumor at 23% (21 of 91 patients) after adenocarcinoma at 34% (31 of 91 patients) that underwent some surgery [Table 1].
The most affected age group was those above 55, at 61.9%, followed by those 36–55 years of age, at 33.33%, and those above 19 but below 36, at 4.76% [Figure 1a].
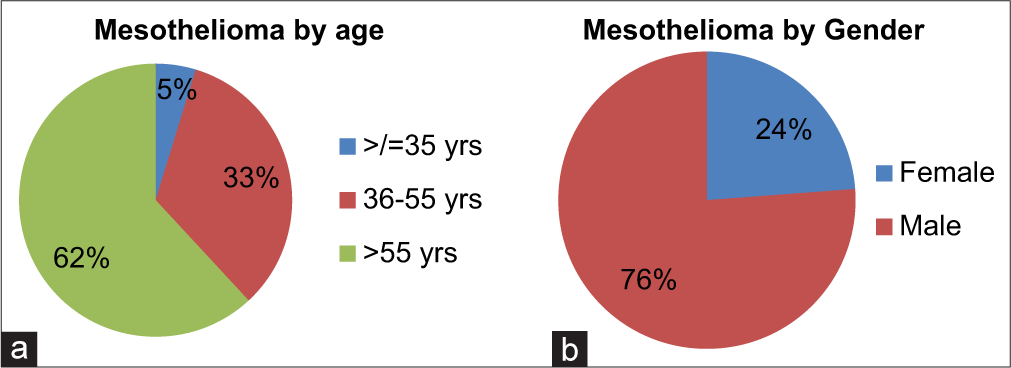
- Breakdown of mesothelioma by (a) age and (b) gender.
Males were diagnosed more than females at 76.19% and 23.81%, respectively [Figure 1b].
About 52.38% of MPM were diagnosed from decortication, 47.62% from pleural biopsy, and none following pulmonary resection and lung biopsy [Table 1].
DISCUSSION
MPM remains challenging and complex in terms of diagnosis, staging, and treatment. An optimal strategy for tackling MPM has yet to be clearly defined.[13] An estimated 200 mesothelioma cases are diagnosed in South Africa (SA) each year.[19,20] The country may have the greatest frequency of malignant mesothelioma worldwide because SA has more than a century of asbestos mining in the Northern Cape, North-West, Limpopo, and Mpumalanga provinces, and this impacts the incidence of the disease.[21] Lack of data, however, may be affecting the demonstration of this increasing incidence and frequency of the disease. In our audit, mesothelioma was the second most frequently diagnosed tumor at 23%. Our audit revealed that 62% of patients diagnosed with MPM were 55 years and older, and 38% were younger than 55 years, which feeds into the fallacy that mesothelioma is a disease of the elderly. This undermines its known long latency period.[22,23] Environmental factors such as exposure to mining dumps, asbestos roofing, and asbestos fibers brought home on family members’ clothing professionally exposed to asbestos may facilitate early exposure, leading to early MPM.[24]
MPM is not a gender-exclusive cancer; however, it affects more men than women, and this is most likely because men have greater likelihood of being exposed to asbestos in their line of work compared to women.[25,26] This was consistent with our findings, where 76% of our patients were males. However, recent studies cite an increase in MPM among women.[22,23] This is critical for reducing gender disparity in diagnosing and caring for MPM. Of interest, those diagnosed with empyema thoracis were patients suspected to be infected with tuberculosis (TB) who subsequently underwent decortication. However, MPM was the confirmed diagnosis and the cause of empyema thoracis in these cases. This is critical in SA, a country with the highest prevalence and incidence of TB, which could be a precursor for misdiagnosis due to the low index of suspicion compounded by the limited access to specialist thoracic surgery services.
MPM does not yet have a recognized cure. The US Food and Drug Administration approved pharmaceutical drugs (Opdivo plus Yervoy) for the first-line treatment for adult patients who will not benefit from surgical treatment.[27,28] In SA, the treatment of mesothelioma generally consists of aggressive surgery, chemotherapy, and radiotherapy; however, there is a high fatality rate: 50% of patients die within a year of diagnosis, and about 2 years for the remaining patients, with few exceptions.[21] Although there are several cancer treatment centers where patients with mesothelioma can access treatment in SA, not all cancer centers have medical professionals with expertise in managing mesothelioma. Considering that MPM is regarded as uncommon, medical professionals can misdiagnose patients and fail to recognize the illness, delaying diagnosis and care.[19,20] Long waiting times are a barrier to accessing care for patients that we refer to the oncology center. By the time patients reached their turn, they either had a poor performance status or had succumbed to the disease.
Ethical and humanitarian issues
MPM is a fatal disease with a poor prognosis, often leaving patients and caregivers in emotional distress despite recent medical advancements.[27,28]
There is a paucity of literature addressing the psychological and social effects of mesothelioma on patients[29] and their families. Despite promising advancements in immunotherapy for MPM, treatment options remain limited, and the prognosis remains poor.[30]
Compounding the situation further is that MPM cases are hugely under-reported in many developing nations, including countries where asbestos mining is rampant. Despite the few attempts, estimating MPM’s global incidence and burden is suboptimal.[11] There is a lack of research examining asbestos exposure and its role in diagnosis exposure by gender in national case lists, leading to under-exploration of gender variations in mesothelioma incidence.[31,32] Considering that mesothelioma nearly always results in death, there is a need for more investment in research aimed at developing effective treatments, as well as facilitating earlier detection and improving access to palliative care.[27,28]
There is also a need to deal with the societal impact, including the terminal care of patients diagnosed with the disease. In SA, the compensation fund has been established through the Compensation for Occupational Injuries and Diseases Act number 130 of 1993, and for the mining industry, specifically, the Occupational Diseases in Mines and Works Act number 78 of 1973 as the Asbestos Relief Trust (ART) and the Kgalagadi Relief Trust, both administered by the ART.[1] Proof of occupational exposure is a requirement to gain access to compensation, which may be cumbersome for those lacking the resources to pursue this administrative hurdle. Compounding the access to compensation challenge is non-occupational asbestos exposure cases asbestos mine dumps close to places of residence and schools with asbestos roofing.[33,34] Such exposure qualifies as a social determinant of health, qualifying it as a social and health justice matter.[1] Of concern is evidence that the affected schools and households with asbestos roofs to date are mainly from previously disadvantaged areas of SA, a reflection of the structural enablers of health inequity.
There is a need to improve access to diagnosis, monitor asbestos mine rehabilitation, and review MPM compensation guidelines. Public health practitioners, policymakers, health communicators, and advocacy groups should make concerted efforts to raise awareness of asbestos exposure risks to society and the role of health professionals in facilitating access to compensation. In SA, mine workers came from all over the country and neighboring countries such as Swaziland, Mozambique, and Zimbabwe. Most workers were poorly educated and may not have understood the risks they were facing then and now, including the high likelihood of not being aware of compensation for occupational diseases.
Limitations
Limitations to this study include the shortcomings of not analyzing patients’ medical records and being limited to the data retrieved from the NHLS laboratory. Therefore, patient-reported information and clinical assessments were not analyzed. The lack of patient admissions data in the form of history of presentations and possible exposure to asbestos presented limitations. The study did not include data generated from other clinical units. It also excluded other thoracic cancers diagnosed outside the cardiothoracic department.
CONCLUSION
The lack of MPM databases worldwide enables under-reporting, which undermines investment in resources to tackle the scourge. The difficulty posed by the disease in terms of diagnosis, treatment, and aftercare of patients qualifies it to be called a scourge. The health inequity contributes to the difficulty with the diagnosis. Poor access to specialized care requires moral reflection. Justice should underpin multistakeholder interventions from policymakers, employers, health experts, and health advocates.
Acknowledgments
We would like to acknowledge National Health Laboratory Services for having availed the histological results to us for this study.
Ethical approval
The research/study was approved by the Sefako Makgatho Health Sciences University Research Ethics Committee, with a clearance certificate number SMUREC/M/434/2022, dated December 01, 2022.
Declaration of patient consent
Patient consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Compensation for environmental asbestos-related diseases in South Africa: A neglected issue. Glob Health Action. 2013;6:19410.
- [CrossRef] [PubMed] [Google Scholar]
- The ticking time-bomb of asbestos: Its insidious role in the development of malignant mesothelioma. Crit Rev Oncol Hematol. 2012;84:200-12.
- [CrossRef] [PubMed] [Google Scholar]
- Update on biology and management of mesothelioma. Eur Respir Rev. 2021;30:200226.
- [CrossRef] [PubMed] [Google Scholar]
- Estimation of the global burden of mesothelioma deaths from incomplete national mortality data. Occup Environ Med. 2017;74:851-8.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of mesothelioma deaths by national income category: Current status and future implications. Int J Environ Res Public Health. 2020;17:6900.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant mesothelioma: New insights into a rare disease. Cancer Treat Rev. 2013;39:584-91.
- [CrossRef] [PubMed] [Google Scholar]
- Global mesothelioma epidemic: Trend and features. Indian J Occup Environ Med. 2014;18:82-8.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of global trends in the diagnosis of mesothelioma from 1990 to 2017. JAMA Netw Open. 2021;4:e2120360.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant mesothelioma: A clinical study of 238 cases. Ind Health. 2011;49:166-72.
- [CrossRef] [PubMed] [Google Scholar]
- Statement on malignant mesothelioma in the UK. Thorax. 2002;57:187.
- [CrossRef] [PubMed] [Google Scholar]
- Global magnitude of reported and unreported mesothelioma. Environ Health Perspect. 2011;119:514-8.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for pathologic diagnosis of Malignant Mesothelioma: 2017 Update of the consensus statement from the International Mesothelioma Interest Group. Arch Pathol Lab Med. 2018;142:89-108.
- [CrossRef] [PubMed] [Google Scholar]
- Second Italian consensus conference on malignant pleural mesothelioma: State of the art and recommendations. Cancer Treat Rev. 2013;39:328-39.
- [CrossRef] [PubMed] [Google Scholar]
- Application of immunohistochemistry to the diagnosis of malignant mesothelioma. Arch Pathol Lab Med. 2008;132:397-401.
- [CrossRef] [PubMed] [Google Scholar]
- Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: Clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol. 2011;12:763-72.
- [CrossRef] [PubMed] [Google Scholar]
- Mesothelioma and radical surgery 2 (MARS 2): Protocol for a multicentre randomised trial comparing (extended) pleurectomy decortication versus no (extended) pleurectomy decortication for patients with malignant pleural mesothelioma. BMJ Open. 2020;10:e038892.
- [CrossRef] [PubMed] [Google Scholar]
- Perspectives on the treatment of malignant pleural mesothelioma. N Engl J Med. 2021;385:1207-18.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant pleural mesothelioma incidence and survival in the Republic of Ireland 1994-2009. Cancer Epidemiol. 2014;38:35-41.
- [CrossRef] [PubMed] [Google Scholar]
- Mesothelioma in South Africa. 2022. Available from: https://www.asbestos.com/mesothelioma/south-africa/#sources [Last accessed on 2024 May 18]
- [Google Scholar]
- What is the survival rate for mesothelioma? 2022. Available from: https://www.asbestos.com/mesothelioma/survival-rate [Last accessed on 2022 Aug 30]
- [Google Scholar]
- UCT Pathology Learning Centre. 2017. Asbestos. Available from: http://www.pathologylearningcentre.uct.ac.za/harmful-substances-asbestos [Last accessed on 2024 May 18]
- [Google Scholar]
- Mesothelioma causes and risk factors. 2022. Available from: https://www.mesothelioma.com/mesothelioma/causes [Last accessed on 2022 Aug 30]
- [Google Scholar]
- Mesothelioma. 2022. Available from: https://www.mesothelioma.com/mesothelioma/prognosis/survival-rate/#:~:text=improving%20mesothelioma%20survival&text=the%20chemotherapy%20wash%2c%20known%20as,rate%20of%2067%25%20or%20higher [Last accessed on 2022 Aug 30]
- [Google Scholar]
- Simian virus 40: The link with human malignant mesothelioma is well established. Anticancer Res. 2000;20:875-7.
- [Google Scholar]
- Risk factors for malignant mesothelioma. 2018. Available from: https://www.cancer.org/cancer/malignant-mesothelioma/causes-risks-prevention/risk-factors.html [Last accessed on 2022 Aug 30]
- [Google Scholar]
- American Cancer Society. 2022. Available from: https://www.cancer.org/cancer/malignant-mesothelioma/detection-diagnosis-staging/survival-statistics.html [Last accessed on 2022 Aug 30]
- [Google Scholar]
- Fact sheet on mesothelioma. 2021. Available from: https://cansa.org.za/files/2021/03/fact-sheet-on-mesothelioma-ncr-2017-web-march-2021.pdf [Last accessed on 2024 May 18]
- [Google Scholar]
- FDA approves drug combination for treating mesothelioma. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-drug-combination-treating-mesothelioma [Last accessed on 2020 Oct 02]
- [Google Scholar]
- What are the psychological effects of mesothelioma on patients and their carers? A scoping review. Psychooncology. 2020;29:1464-73.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and clinical aspects of malignant pleural mesothelioma. Cancers. 2021;13:4194.
- [CrossRef] [PubMed] [Google Scholar]
- Research priorities in mesothelioma: A James Lind Alliance priority setting partnership. Lung Cancer. 2015;89:175-80.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiology of malignant mesothelioma in women: Gender differences and modalities of asbestos exposure. Occup Environ Med. 2016;75:254-62.
- [CrossRef] [PubMed] [Google Scholar]
- A report on asbestos in Gauteng schools. 2017. Available from: https://www.nioh.ac.za/a-report-on-asbestos-in-gauteng-schools/# [Last accessed on 2024 Jul 15]
- [Google Scholar]
- Process to remove asbestos roofs in Free State finally gets underway Republic of South Africa: SABC News; 2024.
- [Google Scholar]







