Translate this page into:
COVID-19 and acute ST-elevation myocardial infarction (STEMI) and ventricular thrombus in a young ethiopian man without known cardiac risk factors: A case report
-
Received: ,
Accepted: ,
How to cite this article: Huluka DK, Birhan YA, Sikamo AP, Getachew N, Meshesha A, Sherman CB. COVID-19 and acute ST-elevation myocardial infarction (STEMI) and ventricular thrombus in a young ethiopian man without known cardiac risk factors: A case report. J Pan Afr Thorac Soc 2022;3:56-8.
Abstract
Patients with coronavirus disease 2019 (COVID-19) can present with pneumonia and acute respiratory distress syndrome but rarely with acute myocardial infarction, especially in the absence of known cardiovascular disease risk factors. We present the case of a previously healthy young Ethiopian man with COVID-19 and no known cardiovascular risk factors who was diagnosed with acute ST-elevation myocardial infarction and left ventricular thrombus.
Keywords
Coronavirus disease 2019
ST-elevation myocardial infarction
LV thrombus
INTRODUCTION
Most of coronavirus disease 2019 (COVID- 19) patients often have mild symptoms or are asymptomatic. Albeit, some patients may present with serious disease including pneumonia and acute respiratory distress syndrome. Patients with traditional cardiovascular disease risk factors like hypertension, diabetes, obesity, male sex, and those with established cardiovascular diseases are considered high-risk patients with increased mortality and morbidity when affected by COVID-19.[1] Cardiovascular system may also be affected by COVID-19 but rarely with acute myocardial infarction, especially in the absence of known cardiovascular risk factors.[2]
CASE REPORT
A 45-year man developed fever, myalgia, arthralgia, and dry cough of 3 weeks duration. He was evaluated and thought to have typhoid or typhus; he was treated with Ciprofloxacin and Doxycycline. He failed to improve and twelve days prior to admission, his cough became more productive; a chest x-ray showed lower lobe infiltrates. His antibiotics were switch to Augmentin and Azithromycin. A RT PCR COVID-19 test was obtained and subsequently recorded as positive. Five days prior to admission and while still on home isolation, he experienced chest tightness, exertional fatigue, and anorexia. His symptoms persisted and he visited a different clinic. Investigations revealed WBC 14,200/mm3 (n = 67.7%, L = 11.4%) and troponin 18.16 ng/ml (normal: 0.0–0.3 ng/ml). His lipid profile, fasting blood sugar, hemoglobin A1C, electrolytes, and renal function were all normal. His chest x-ray showed mild bibasilar ground-glass opacities and his ECG revealed ST elevation and Q waves in the inferior leads with reciprocal changes in the lateral leads [Figure 1]. Echocardiography was remarkable for inferior wall hypokinesis and LV thrombus with an EF of 40–45%. He was then referred to Eka Kotebe General Hospital, one of the COVID-19 care centers in Addis Ababa.

- ECG showing ST elevation and Q-waves in inferior leads with reciprocal changes on the lateral leads.
On admission, he lacked all the traditional risk factors for ischemic heart disease. His physical exam was remarkable only for BP: 120/70 mmHg, PR 100 bpm, and SaO2 89-92% on room air. He was treated with aspirin, clopidogrel, enoxaparin overlapping with warfarin, and supplemental oxygen. Angiography, done after discharge, showed occlusion of the left anterior descending and right coronary arteries [Figure 2]. He subsequently had percutaneous coronary intervention (PCI) and is currently asymptomatic.
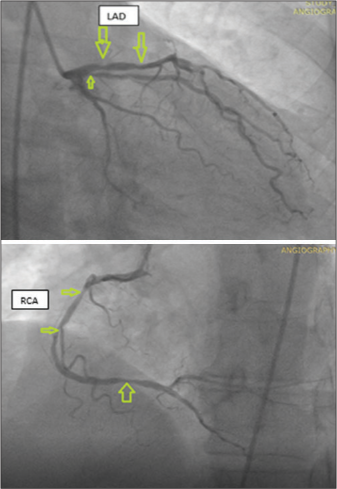
- Coronary angiography showing stenotic lesions in the left anterior descending artery (LAD) and multisite (proximal, mid, and distal) stenotic lesions of the right coronary artery (RCA).
DISCUSSION
Even though respiratory manifestations are the predominant manifestation for COVID-19 illness, COVID-19 can either induce new cardiac pathologies and/or exacerbate underlying cardiovascular diseases.[2] It can affect the cardiovascular system by different mechanisms including direct myocardial damage, severe systemic inflammatory response, hypoxia, right heart strain secondary to ARDS and lung injury, and plaque rupture secondary to inflammation.[3]
Our patient had typical features of an acute ST-elevation myocardial infarction (STEMI), namely chest pain, ECG changes, elevated cardiac biomarkers, and echocardiographic and angiographic evidence of coronary artery disease. He developed cardiac symptoms 2 weeks after his initial symptoms and 06 days after COVID-19 RT-PCR positivity. However, he was lacking known risk factor for ischemic heart disease. COVID-19 was likely responsible for his STEMI, possibly mediated by inflammation and/or hypercoagulation.[2-4] This case underscores the need for clinicians to consider further cardiac evaluation in COVID-19 patients presenting with chest pain, regardless of age or lack of known cardiovascular risk factors other than being male.
In this particular patient diagnosis of COVID-19 has contributed significantly for the delay in the diagnosis of STEMI and timely guideline-based interventions. A joint position Statement from the society for cardiovascular angiography and interventions, the American College of Cardiology, and the American College of Emergency Physicians emphasizes that primary PCI should remain the standard of care, including for COVID-19 confirmed or probable patients.[5] However, there is a significant delay in hospital presentation of STEMI patients because of the fear of nosocomial COVID-19 transmission.[6] There is also a delay in door to balloon time after hospital presentation especially for COVID-19 suspected/confirmed cases due to logistic issues to facilitate Cardiovascular procedures in the safest possible environment to optimize clinical outcomes and minimize the risk of infection. Fortunately, our patient did well but because COVID-19 patients are treated at COVID-19 treatment facilities with no PCI capacities in Ethiopia there was a delay in PCI intervention.
Acknowledgment
We would like to pass our gratitude to the East African Training Initiative, sponsored by Vital Strategies New York, New York, USA, and the Swiss Lung Foundation, Zurich, Switzerland.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-9.
- [CrossRef] [PubMed] [Google Scholar]
- Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020;5:831-40.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 Pandemic: Cardiovascular complications and future implications. Am J Cardiovasc Drugs. 2020;20:311-24.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation, immunity, and infection in atherothrombosis: JACC review topic of the week. J Am Coll Cardiol. 2018;72:2071-81.
- [CrossRef] [PubMed] [Google Scholar]
- Management of acute myocardial infarction during the COVID-19 pandemic: A position statement from the society for cardiovascular angiography and interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicia. J Am Coll Cardiol. 2020;76:1375-84.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of coronavirus disease 2019 (COVID-19) outbreak on st-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631.
- [CrossRef] [PubMed] [Google Scholar]






